When the head tilts in the roll plane (ear to shoulder, about the front to back axis), the resultant angular acceleration drives the semicircular canals resulting in phasic torsional eye movements.
However, when there are changes in the orientation of the head relative to gravity, and with a sustained lateral tilt, the eyes counter-roll in the opposite direction to the head tilt. This static change in torsion is driven by inputs from the otoliths (mainly the utricle), which sense the pull of gravity1. The otolithic input serves to maintain a constant, unaltered position of the eyes in space (gaze).
The reflex driven by the otoliths includes the generation of:
- Torsional eye movements during head roll (counterrolling) or
- Vertical eye movements during head pitch (counterpitching)2.
Normally, when stationary, balanced signals from the utriculo-ocular pathway are used to align the head’s vertical axis and the eye’s vertical meridian with absolute earth-vertical (gravity). For example, when the head is tilted counterclockwise, the eyes compensate for the head tilt by rotating clockwise, so that the eyes’ vertical meridian is realigned with earth-vertical. At the same time, the right eye depresses and the left eye elevates, so that the eyes’ horizontal meridian is realigned with earth-horizontal3.
Damage to the utriculo-ocular pathway lead to an erroneous internal estimate of absolute earth-vertical (gravity); that is, the brain erroneously computes that the head is tilted, despite the fact that the head may actually be in an upright position and that the utricles are still in the horizontal plane.
Thus, a lesion that decreases innervation from the left otolith (resulting in a pathologic relative increase in innervation from the right otolith) will drive the head tilt and generate a left head tilt, elevation and intorsion of the right eye, and depression and extorsion of the left eye (left ocular tilt reaction). This triad of head tilt, skew deviation, and abnormal torsion seen in the ocular tilt reaction (OTR) represents a righting response, the goal of which is to realign the vertical axes of both the head and the eyes to the internal estimate of absolute earth-vertical, even though this estimate is faulty.
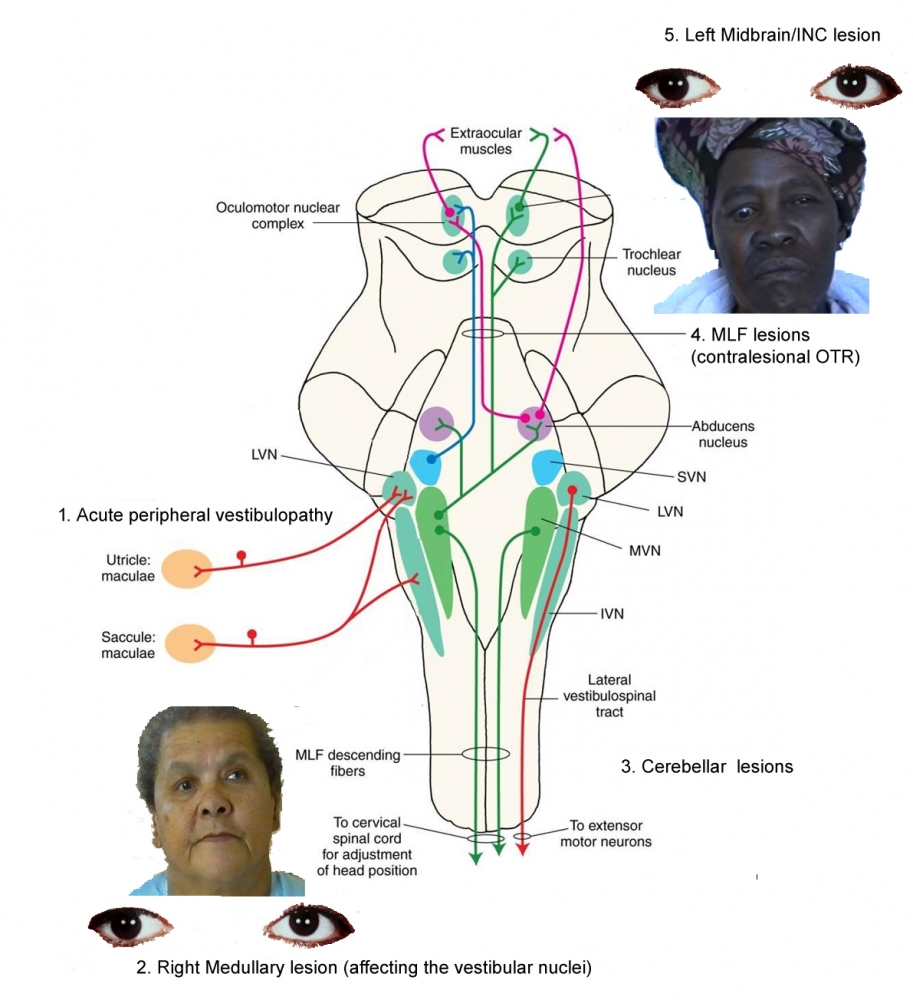
The physiological OTR depends on a crossed graviceptive (ie, sensitive to gravity) pathway which arises from excitation of the dependent utricle, and then projects via the ipsilateral vestibular nucleus to the contralateral interstitial nucleus of Cajal (INC) and then on to oculomotor and spinal motor neurons5.
The utriculo-ocular motor fibers which carry signals from the vestibular apparatus will decussate at the level of the pontomedullary junction and ascend as part of the contralateral MLF. The fibres reach the midbrain to supply the 3rd and 4th nuclei, as well as the INC6.
1. OTR (Ocular Tilt Reaction)
Brainstem lesions which affect the vestibular system in the roll plane give rise to symptoms and signs in three modalities9:
- Oculomotor: skew deviation and ocular torsion
- Perceptual: deviation of subjective visual vertical (SVV)
- Postural: lateropulsion of the body
The OTR reflects an imbalance analogous to the spontaneous nystagmus that occurs when there is a tone imbalance between the semicircular canals in each labyrinth7. In that case there is a static semicircular canal pathway imbalance, whereas in the case of the OTR, there is a static utricular pathway imbalance.
By definition, a rightward OTR comprises a:
- Rightward head tilt
- Right skew deviation (ie, a right hypotropia)
- Rightward eye torsion (counterroll): Torsion of both eyes with the top poles rotating toward the side of lower eye (ie, excyclotorsion of the right eye and incyclotorsion of the left eye).
- Deviation of the subjective visual vertical to the right, a perceptual tilt of the visual world to the right.
Details of the eye movements seen in a right OTR are:
-The left eye elevates from contraction of the left superior rectus (decussating fibers from the right third nucleus), and incyclotorts from contraction of the right superior oblique (decussating fibers from the left fourth nucleus).
-The right eye depresses from contraction of the right inferior rectus (fibers from the right third nucleus), and excyclotorts from contraction of the left inferior oblique (fibers from the left third nucleus).
-Afferents from the utricle ascending in the right MLF will synapse in the right interstitial nucleus of Cajal, which is responsible for vertical and torsional gaze-holding. This ensures that the eyes will stay in the desired position while the head tilt is maintained.

Redrawn from: Brandt T, Dieterich M. Vestibular syndromes in the roll plane: topographic diagnosis from brainstem to cortex. Ann Neurol. 1994;36(3):337-47.
Lesions giving rise to an OTR typically involve:
- The peripheral labyrinth: peripheral lesions cause an ocular tilt and SVV of similar direction and magnitude. By contrast, central vestibular lesions may have differences between the ocular tilt and the SVV due to different involvement of the particular pathways, with a tendency for the SVV to be more frequent and more pronounced8.
- The vestibular nerve and the vestibular nucleus in the medulla, as in a lateral medullary syndrome, results in an ipsiversive OTR (eye down on the side of the lesion).
- The MLF in the pons or caudal midbrain, including the INC: the commonest brainstem lesions resulting in an contraversive OTR are caused by damage to the vestibular nuclei projections which ascend to the ocular motor nuclei via the MLF1: this causes a contralateral OTR: that is, hypotropia and excyclorotation of the eye contralateral to the MLF lesion.
- A left MLF lesion results in a right OTR with head tilt to the right, hypotropia of the right eye, counterroll of both eyes (top poles) towards the right ear, and SVV tilted to the right.
- A right MLF lesion results in a left OTR with head tilt to the left, hypotropia of the left eye, counterroll of both eyes (top poles) towards the left ear, and SVV tilted to the left.
- Skew deviations may also occur with cerebellar lesions; the eye which is higher will alternate depending on whether the gaze is directed to the left or right. Usually the abducting eye is higher.
2. TILT OF THE HEAD
Tilt of the head toward the right or left shoulder is observed in patients with:
- Superior oblique palsy: the head is tilted towards the non-affected side to lessen diplopia.
- An ocular tilt reaction (OTR) due to a imbalance of the VOR in the roll plane10. In the OTR the head is tilted to the side of the lower eye.
Depending on the side of the tilt, the lesion will be either ipsilateral or contralateral:
- On the side of the tilt: lesion is ipsilateral to the side of tilt. For example, an acute unilateral peripheral vestibular lesion or an acute unilateral central lesion in the medulla oblongata (eg, in Wallenberg’s syndrome)
- On the side opposite to the side of the tilt: lesion is contralateral to the side of tilt. For example, pontomesencephalic lesions, commonly in the MLF. The otolith-ocular pathway crosses at the level of the vestibular nucleus such that with lesions above the decussation, the higher eye is on the side of the lesion (as in internuclear ophthalmoplegia).
Pontomedullary lesions cause ipsilateral SVV tilts, whereas pontomesencephalic lesions cause contralateral SVV tilts.
The graviceptive pathways cross at the level between the vesibular and abducens nuclei.
3. SKEW DEVIATION
Skew deviation is a vertical misalignment of the visual axes caused by a disturbance of supranuclear inputs as a result of lesions in the brainstem, cerebellum, or peripheral vestibular system (ie, the inner ear and its afferent projections). The vertical misalignment may be comitant or incomitant. Rarely, it alternates with eye position (eg, right hypertropia on right gaze and left hypertropia on left gaze).
Skew deviation is the hallmark of an imbalance in the tonic levels of activity underlying otolith-ocular reflexes, and is a naturally occurring component of the reflex balance and postural responses which occur in lateral-eyed animals, (ie, rabbits) in response to lateral tilt of the body in order that they can keep their eyes aligned with the horizontal meridian and the head and body upright. Presumably in frontal-eyed animals (ie, humans) this pattern of eye deviation only emerges when otolith inputs become unbalanced in a non-physiological manner. Patients with a skew deviation may complain of a vertical and sometimes torsional diplopia.
Skew deviation is often the initial manifestation of diseases that affect the brainstem, cerebellum, or peripheral vestibular system11. Rare causes include raised intracranial pressure and paroxysmal skew in the case of seizures involving vestibular cortex12.
Acutely, torsional nystagmus is commonly also present.
Skew deviation may be detected by alternate cover testing. With the alternate cover test, a vertical corrective movement on switching the cover from one eye to the other is looked for, indicating vertical misalignment.
The effect of the position of the eye in the orbit and of left and right head tilt on the skew should also be recorded, particularly to exclude a 4th nerve palsy. In contrast to a 4th nerve palsy, the vertical misalignment in skew deviation does not typically follow any set patterns; although usually comitant ( as opposed to superior oblique palsy), it may be non-comitant, or may even alternate with gaze direction.
Note that vertical misalignment in skew decreases by at least 50% when patients changed from an upright to a supine position ( a helpful feature to distinguish skew from superior oblique palsy)11.
4. SUBJECTIVE VISUAL VERTICAL (SVV)
Normally, the subjective visual vertical (SVV) is aligned with the gravitational vertical13. A tilt of the SVV is a sensitive sign of a disturbance in the otolith-ocular pathways, and indicates vestibular tone imbalance in the roll plane11.
Furthermore, body lateropulsion is correlated with SVV tilt, ie, the more pronounced the lateropulsion, the greater the SVV tilt14.
Tilt of the SVV occurs in lesions of central and peripheral vestibular pathways, and, in particular, is seen in the majority of patients with acute unilateral brainstem lesions that affect the central graviceptive pathwaysrunning from which run from the vestibular nuclei via the medial longitudinal fasciculus to the midbrain4. For example, marked image tilting (ranging from 90 to 180 degrees) may be seen in the lateral medullary syndrome.
On the two extremes: thalamocortical lesions and peripheral vestibular lesions:
- Lesions of the more rostral pathways, including the thalamus and notably the cortex in the posterior region of the insula, will produce the same disturbance of the SVV. In thalamic lesions, the tilts of SVV may be contraversive or ipsiversive; in vestibular cortex lesions they are most often contraversive. Note however, that an OTR is not induced by supratentorial lesions above the level of the INC16.
- Most patients with acute vestibular neuritis show a small and transient ipsilateral deviation of the SVV, but brainstem lesions can produce larger and longer lasting tilts of the SVV.
In the rostral medullary tegmentum and caudal pons the tilt of the SVV is ipsilateral to the lesion.
In the rostral pons and caudal mesencephalic tegmentum the tilt of the SVV is contralateral to the lesion.
The SVV can be measured at the bedside using the bucket method15. The subject estimates verticality by aligning a dark straight line visible on the bottom of a bucket that is rotated to the right or left by the examiner. On the outside, there is a plumb line on the bottom of the bucket that originates from the center of a semicircle divided into degrees with the zero line adjusted to the dark line inside. In this way the deviation from true vertical can be measured by averaging a few trials.

Redrawn from: Zwergal A, Rettinger N, Frenzel C, Dieterich M, Brandt T, Strupp M. A bucket of static vestibular function. Neurology. 2009;72(19):1689-92.
4. OCULAR COUNTER ROLL
Ocular counter-roll is difficult to detect clinically without photography; however, if there is a large amount of counter-roll, it can be shown by the tilt of the imaginary line that connects the macula with the optic disc.
In most skew deviations, except for those caused by a lesion in the lateral medulla, ocular torsion is binocular and conjugate (ie, excyclotorsion of the hypotropic eye and incyclotorsion of the hypertropic eye).
In patients with lateral medullary syndrome, the ocular torsion is monocular (ie, the hypotropic eye is excyclotorted, but the hypertropic eye has normal torsion or is slightly incyclotorted)11. The pathological ocular counter-roll arising in an OTR is signficantly greater than the normal counter-roll6.
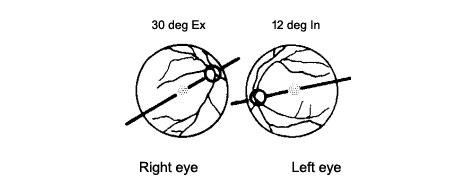
Redrawn from: Dieterich M, Brandt T. Ocular torsion and tilt of subjective visual vertical are sensitive brainstem signs. Ann Neurol. 1993;33(3):292?299. doi:10.1002/ana.410330311