In general, clinical ability to distinguish one type of SCA from another based on oculomotor findings is not particularly accurate1.
SCA 1
Vestibulo-ocular reflex (VOR) gain is low, in addition to abnormal smooth pursuit.
Saccade slowing, dysmetria, and increased latency may be present2. Saccade slowing is likely related to lesions of the generators of saccades within the brainstem (PPRF, riMLF).
SCA 2
Patients have early, and relatively marked slowness of horizontal saccades. Vertical saccades are also impaired. This may progress to a complete saccadic paresis and complete external ophthalmoplegia (complete gaze palsy horizontally and vertically).
Slowing of saccade velocity strongly correlates with the polyglutamine expansion, but it is inversely correlated with the severity of ataxia3. There is no correlation between the duration of the disease and saccade slowing, which may be present even before manifestations of other clinical features of the disease. Saccade velocity is a sensitive and specific marker of disease activity.
Absence of gaze evoked nystagmus (GEN) or dysmetric saccades in these patients has a high negative predictive value for the presence of SCA 24, likely due to that fact that correct saccade generation is necessary to evoke GEN1.
MRI demonstrates a reduction in the size of cerebellum, but also of pons and midbrain, and saccade slowing may not arise as a result of cerebellar dysfunction, but due to impairment of the burst neurons in the brainstem.
SCA 3
SCA3 is clinically characterized by a high frequency of blepharospasm and ophthalmoparesis.
Saccadic dysmetria is present, with low velocity of saccades, and overshoot.There is limited upgaze.
Impaired smooth pursuit and optokinetic nystagmus are present.
GEN is present.
There is horizontal VOR dysfunction, with a low VOR gain1.
Degenerative changes in mesencephalic neurons may be responsible for the reduced saccade velocity due to deficient burst generation2.
SCA 6
Symptoms of vertigo and dizziness occur in the majority of patients5. Downbeat nystagmus (DBN), vertical positional nystagmus, as seen in positioning maneuvers, and abnormal head-shaking nystagmus (vertical nystagmus elicited by horizontal head shaking) are pathognomonic1.
VOR gain may be elevated above normal in the early stages of the disease, and is often easiest to document using video head impulse testing6.
(vv)SCA6.mp4(tt)
From: Zee DS. The cerebellum for the neuro-ophthalmologist: A video tutorial of some signs and syndromes to recognize NANOS 42nd Annual Meeting 2016.
Retrieved from: https://collections.lib.utah.edu/ark:/87278/s6nw2r5g
SCA 7
The disorder is characterized by retinal degeneration and ophthalmoplegia7.
Oculomotor findings include nystagmus, saccadic intrusions, saccadic hypo- and hypermetria, slow saccades, impaired smooth pursuit and VOR cancellation, and late in the illness, ophthalmoparesis and ophthalmoplegia.
Anti-GAD antibody
Eye movement abnormalities include:
DBN
Slow vertical saccades, prolonged saccade latency, and saccadic hypometria and dysmetria.
Loss of downward smooth pursuit, and impaired cancellation of the VOR.
Saccadic oscillations including opsoclonus.
Pathogenesis:
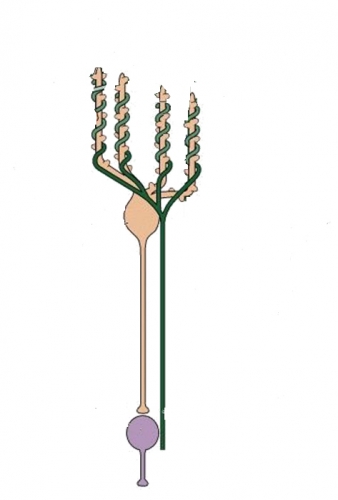
The frequent interruptions of ongoing saccades, but normal velocity of each “broken” saccade segment suggests impaired programming leading to hypometria, a classic cerebellar phenomenon. Slowing of saccades may also suggest involvement of burst generators.
There may also be an overall increase in burst neuron excitability due to decreased degradation of gluatamate to GABA, resulting in an unstable reciprocally innervating circuit of burst neurons, causing opsoclonus2.