Genetics
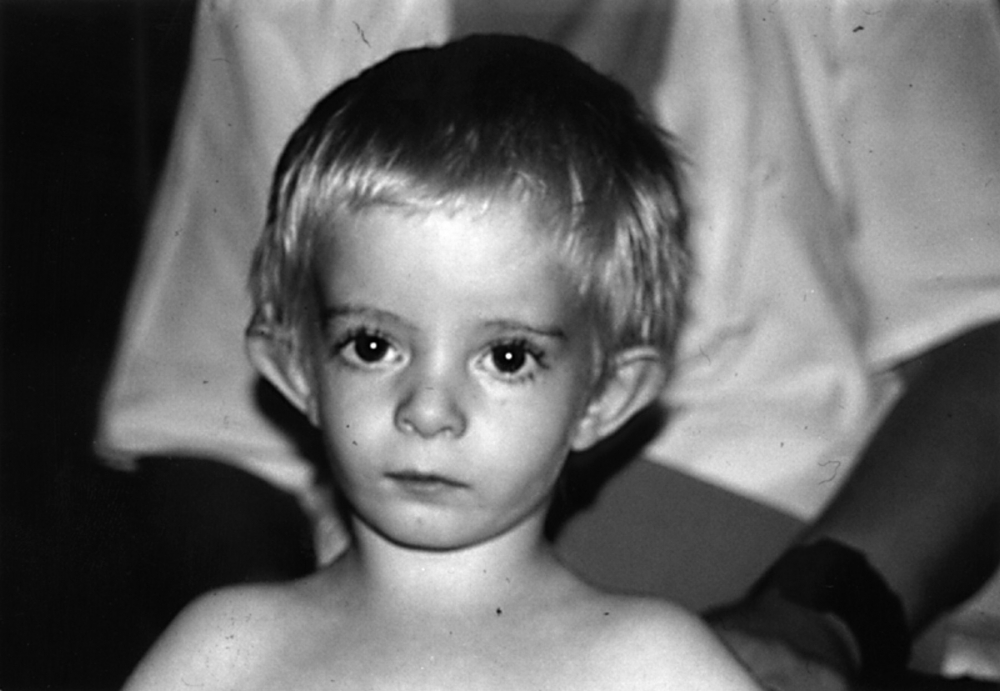
In myoclonus–dystonia (MD) (formerly referred to as DYT11), the features of two different movement disorders are combined. Many kindreds with autosomal dominantly inherited myoclonus dystonia have mutations in the gene for epsilon sarcoglycan (SGCE). About 80 different mutations have been reported in SGCE, many of which are loss-of-function mutations due to frameshift, splice site, nonsense mutations, or deletions of whole exons or even the entire gene.SGCE mutations have reduced penetrance of maternally transmitted mutations as a result of maternal imprinting of the SGCE gene which causes selective methylation of CpG dinucleotides within the promoter region of the gene of the maternal allele, with expression of the paternal allele only1. Patients with myoclonus-dystonia may have maternal duplication of chromosome 7 (Silver-Russell syndrome), characterised by gross deficiency, and typical facial appearance2.
Clinical features predictive of the presence of the SGCE mutation include1:
- Myoclonus as prominent sign, predominantly upper body
- Positive family history
- Psychiatric comorbidities (phobia, OCD, alcohol dependence)
Pathogenesis
The disorder is held to be a dysfunction of cerebellar-thalamus pathways. Electrophysiological testing appears to indicate that the myoclonus is not of cortical origin.
Mode of Inheritance
Mutation-positive patients present in childhood or adolescence, predominantly with myoclonus. The disorder occurs before age 10 in the vast majority of patients whereas onset after age 20 is very
unusua2l. The SGCE gene undergoes maternal genomic imprinting, so that only 10% of patients who inherit a mutated maternal gene will express the disorder, and a family history may therefore not be apparent. This impacts on genetic counselling since it is very unlikely that offspring who inherited the mutation from the mother will develop the disease because only the wildtype allele from the father will be expressed and the mutated, maternal allele will be inactive due to the imprinting mechanism3.
Furthermore, genetic heterogeneity in present, in that some patients with the clinical presentation of myoclonus-dystonia do not have SGCE gene mutations4.
Additionally, many carriers of SGCE mutations develop psychiatric features such as anxiety-related disorders and alcohol dependence.
Clinical Presentation
Movement
The initial symptoms at the onset of MD emerge in childhood and usually consist of lightning jerks and dystonia mostly affecting the neck and upper limbs, with predominantly proximal involvement and slow progression5. The disease course is typically fairly benign1. Dystonia may remit in a minority of cases.On the other hand, motor disorders may significantly impair quality-of-life and restrict ADLs2.
• Dystonia usually occurs later and remains mild, although exceptions occur. Dystonia occurs in about two-thirds of patients, usually in the form of mild cervical dystonia and writer’s cramp. Dystonia may also affect the larynx and lower limbs (especially in paediatric patients5).Usually the face, larynx and trunk are spared2.
• The myoclonic jerks typically are brief, lightning-like and predominantly affect the neck, trunk and upper limbs. The jerks are action-induced and alcohol-responsive, and likely are a relatively specific (and hence useful) physical sign to rule in the diagnosis of MD. Myoclonus tends predominantly to be proximal, and may manifest as proximal myoclonus or axial jerks with less involvement of the moving body part2.
In a subset of patients, MD presents as a gait disorder with lower limb onset and evolves into the typical clinical presentation later, during adolescence.
Myoclonus and dystonia are strikingly alleviated by alcohol in many but not in all patients, and similarly, a response to alcohol is not specific for the condition.
Some patients may present with tremor, clinically resembling high frequency myoclonic jerks5.
Psychiatric
Psychiatric comorbidity is common, especially social and other phobias, and obsessive compulsive disorder.There is a significant risk of alcoholism, either related to self treatment, or possibly due to a genetic predisposition2.Currently it is accepted that the psychiatric disorders most likely reflect an alteration of brain function due to the genetic disorder rather than a secondary response to the disability2.
Treatment
Typically, a wide range of medicines have been shown to be of little value:this includes benzodiazepines, valproate, gabapentin, levetiracetam and anticholinergic agents.
There are reports on improvement with levodopa and tetrabenazine. Zonisamide and sodium oxybateHave both been reported in trials to show improvement.
DBS is likely effective6. The target is typically either GPi or VIM. Myoclonus is likely to improve to a greater extent than dystonia.

