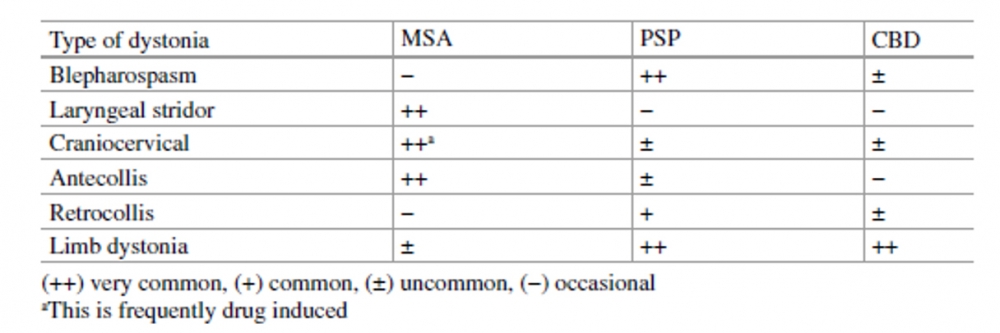
Dystonia is often present in Parkinson-plus syndromes, such as multiple system atrophy (MSA), progressive supranuclear palsy (PSP), and corticobasal degeneration (CBD).
From: Kanovsky P, Bhatia KP, Rosales RL. Dystonia and Dystonic Syndromes. (Kanovsky P, Bhatia KP, Rosales RL, eds.). Vienna: Springer Vienna; 2015. doi:10.1007/978-3-7091-1516-9
MSA
Dystonia is a common feature of MSA, occurring in almost half of cases, and may frequently be present at presentation, notably facial dystonia may be an early sign of the condition.
Various types include:
-Pisa syndrome
-Anterocollis
Disproportionate anterocollis is considered a characteristic feature of this disease, and may be the presenting symptom.
-Laryngeal Stridor
Inspiratory stridor, particularly at night, is commonly attributed to vocal cord paralysis, though it might also reflect dystonia of the vocal cords.
-Limb Dystonia
Limb dystonia in MSA includes dystonic arm posturing, task-specific dystonia (such as writer’s cramp), or equinovarus foot posturing. Limb dystonia is most likely to occur in MSA subjects who are levodopa naïve and tends to improve with dopamine therapy.
PSP
-Limb Dystonia
Limb involvement is the most common dystonic manifestation of PSP patients. Hemidystonia may be a very early feature of this disease in some patients and can lead to a diagnosis of CBD because of the pronounced unilateral dystonia. Single limb involvement is described in 10 % of PSP cases, with the arm being the limb affected most often.
-Blepharospasm
This is well known to occur in PSP; up to 50% of PSP patients with blepharospasm may display apraxia of eyelid opening. However, blepharospasm is typically a late manifestation of the disease. By contrast, apraxia of eyelid opening or closing frequently appears in the middle stages of the disease.
-Retrocollis
Retrocollis associated with axial rigidity is most typically seen in patients with the classic variant of PSP (Richardson’s syndrome). Some authors do not consider this neck posture to be dystonic, since, it is not associated with muscle hypertrophy nor can it be relieved by a geste, both being typical features of classical cervical dystonia.
Laryngeal dystonia may also occur, potentially causing confusion with MSA.
CORTICOBASAL DEGENERATION
A number of pathological substrates that may underlie corticobasal syndrome (CBS) include a wide range of pathologies, such as PSP, Alzheimer’s dementia, Pick’s disease, frontotemporal lobar degeneration with ubiquitin- and TDP-43- positive inclusions, Lewy body disease, frontotemporal lobar degeneration with fused-in sarcoma-positive inclusions, and Creutzfeldt-Jakob disease.
The majority of early-onset dystonic CBD patients display a CBS phenotype, while the remainder have a PSP phenotype.
The majority of patients with late-onset dystonic CBD display a “dementia” phenotype (FTD, AD, or progressive nonfluent aphasia).
Initial distribution of dystonia is typically in the upper limbs, which are usually affected most severely, followed by cervical dystonia and blepharospasm, with a few cases presenting with lower limb dystonia (which is associated with CBS and is usually levodopa induced and reversible).
Upper limb dystonia is more often associated with the CBS phenotype, while cervical dystonia and blepharospasm are more common in other phenotypes, particularly in PSP. Dystonia in CBS associated with CBD appears to occur early in the course of the disease; it is initially most commonly focal (upper limb), and it then progresses to hemidystonia and may subsequently also affect the other side but rarely begins in the leg. Cervical dystonia and blepharospasm are rarely isolated. The typical clinical distribution of dystonia in CBD is adduction and flexion of the arm, forearm, wrist, and metacarpophalangeal joints, extension of the interphalangeal joints, as well as internal rotation and flexion of the hip, flexion of the knee, and inversion of the foot.

