Physiology of Saccades: Pulse and Step Excitatory Burst Neurons in Superior Colliculus and Brainstem
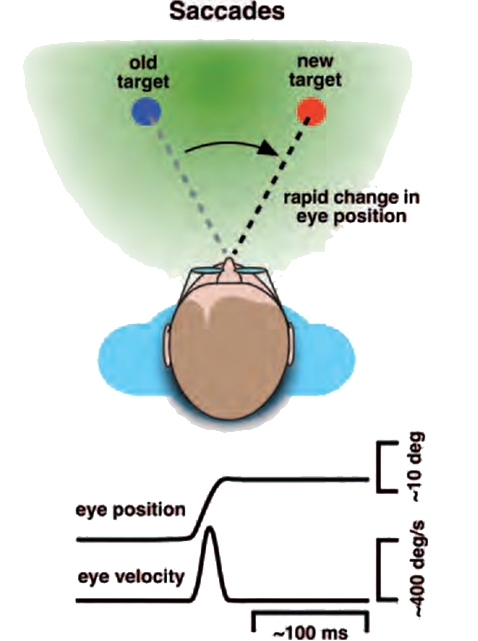
The main function of saccades is to bring new images of interest on to the fovea1. The fovea, the central area of the retina that enables the best visual acuity, is very small (20 in diameter), so saccades need to be very accurate. To minimize interference with vision, saccades must be of very short duration, usually less than a tenth of a second (typically≈30–100 ms) and are the fastest eye movements, with speeds as high as 700°/s, being so fast that vision is blurred as the saccade takes place.
Saccades are ballistic, ‘preprogrammed’, movements, meaning that the desired result of a new eye position is translated into a command, not dependant on feedback. Therefore, saccade speed is not under voluntary or visual control, but depends on the calculated size of the movement, with larger saccades having higher velocities2. Human saccades follow a target jump within ≈250 ms, and stop abruptly (ie, with little subsequent ocular drift). Saccades made to target jumps >100 in amplitude often undershoot the target by ≈10% (saccadic hypometria) , and, after a short latency (≈150 ms), are followed by a corrective saccade2.
Of note, the overwhelming majority of saccades have magnitudes of 15 degrees or less, and are less than 60 ms in duration, corresponding well to clinical assessment of the saccadic system3. A small degree of overshooting (hypermetria) tends to occur with small amplitude saccades4.
Saccades include:
- Eye movement directed to a target (visually guided saccades)
- Voluntary re-fixations to remembered targets (memory guided saccades)
- Involuntary eye movements to novel images (reflexive saccades)
- Eye movements in the opposite direction of a target (antisaccades)
- The quick phases of vestibular and optokinetic nystagmus
- Rapid eye movements of sleep.
The saccadic apparatus includes neurons in the saccade subregion of the frontal eye field (FEFsac) which project to a number of subcortical structures that serve to mediate rapid gaze shifts to remembered targets. Cortical areas and the basal ganglia are important for making saccades, but are more involved in target selection than saccade generation5. This circuitry has a strong influence over saccadic initiation by direct connections with the superior colliculus (SC) and via connections with the caudate nucleus. In addition, the cerebellum is important for maintaining saccade accuracy and for adaptation2.
Together, the FEFsac and SC form an obligatory route for saccadic commands originating in the cerebrum. A lesion of both the FEFsac and SC, but not either alone, causes long-lasting saccadic paralysis. A lesion of either the FEFsac or the SC alone causes subtle abnormalities: mildly hypometric and delayed (increased latency) saccades2.
Each FEFsac and SC generates contralateral horizontal saccades, whereas vertical and torsional saccades are generated by simultaneous activation of both FEFs or both SC.
Superior Colliculus
Information processing in the SC is important for projection to the brainstem centres that mediate eye movements and for the execution of accurate contralateral saccades with horizontal and vertical components.
The SC receives visual information from the retina and striate cortex concerning the contralateral hemifield. The deeper layers of the SC are primarily related to eye movements, but they also contain representations of the body surface and location of sound in space2.
In addition to receiving inputs from the frontal cortex, the superior colliculus receives powerful inhibitory inputs from the substantia nigra pars reticulata of the basal ganglia, which need to be suppressed before the SC can drive a saccade. In a saccade, when the SC determines that the new eye position is equal to the position desired by the visual system, the drive to the oculomotor muscles is switched off, and the eye comes to rest on the new target. Final feedback is provided by the visual system which determines whether the saccade was in fact successful in landing on the target.
The SC projects to the paramedian pontine reticular formation (PPRF) for horizontal saccades, and to the riMLF for vertical saccades.
Frontal Eye Field and Parietal Cortex
The saccade subregion of the frontal eye field (FEFsac), the supplementary eye field, and the dorsolateral prefrontal cortex, as well as the parietal eye field (PEF) and area 7a in the parietal cortex, participate in the control of saccades. These areas initiate saccades by sending trigger signals to the omnipause neurons in the pons, and they encode saccade amplitude and direction. The FEFsac has a powerful two-pronged effect on the superior colliculus: one direct, and the other through the basal ganglia (ie, the caudate and SN pars reticulata)2. The direct frontal eye field projection runs through the anterior limb of the internal capsule to the PPRF and riMLF.
The parietal cortex has a direct projection to the SC. In contrast to the FEF, the parietal cortex is more involved in the production of saccades to novel visual stimuli rather than to remembered targets. Hence, an important dichotomy between the frontal and parietal lobes:
- Internally generated voluntary saccades in the frontal lobes.
- Externally generated reflexes saccades in the parietal lobe.
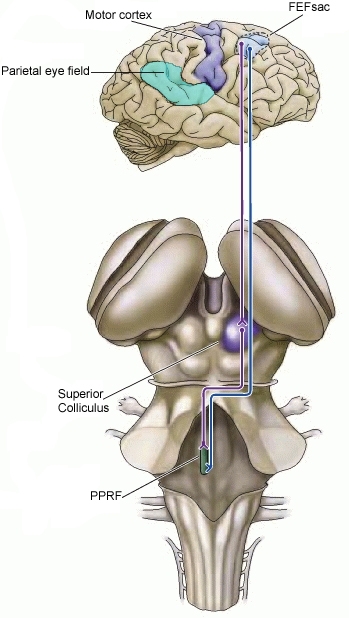
From: Purves D, Augustine GJ, Fitzpatrick D, et al.Available from: https://www.ncbi.nlm.nih.gov/books/NBK10992/ / Public domain
The underlying mechanism for saccades requires a pulse and step command to the motoneurons controlling eye movements. Excitatory burst neurons, which provide the pulse, are located in the PPRF for horizontal saccades, and, for vertical and torsional saccades, in the riMLF in the mesencephalic reticular formation. When no saccade is being generated, burst neurons are tonically inhibited by glycinergic omnipause neurons in the caudal pontine nucleus raphe interpositus, which lies within the PPRF.
The pulse initiates the saccade with a burst of high-frequency, phasic innervational activity that enables the globe to overcome inertia and the viscous drag of the orbit (gaze initiation). The step consists of tonic innervational activity that continues after the saccadic eye movement is complete in order to hold the eye in its new eccentric position against elastic forces in the orbit (gaze holding). The pulse determines saccade velocity, and the step maintains the position of the eye after the saccade. For the saccade to be accurate, the velocity of the saccade (pulse innervation) must match the final ocular position maintained after the saccade is complete (step innervation). The process of matching the pulse and step components of a saccade is referred to as neural integration.
Saccadic eye movements are fine-tuned by the cerebellum, which receives neural input from the pons and supplies innervation to the PPRF and riMLF. The cerebellum influences saccadic speed and accuracy and assists in neural integration (pulse–step matching).
The flocculus and paraflocculus are important for the adaptation of the pulse and pulse-step mismatch for saccades, and lesions of this region lead to post-saccadic drift 2.
Note that saccades and the quick phases of nystagmus are generated by the same brainstem systems6. Once the saccade has been initiated, the retinal target error which determines the required eye position signal is the determining factor for the duration of firing by the excitatory burst neurons which generate the appropriate pulse of activity in the ocular motoneurons2.
Since the cerebral cortex is primarily involved in higher-order, “executive” control of saccades, damage to cortical areas may result in abnormal volitional saccades.
Damage to the cerebellum (dorsal vermis & fastigial nucleus) causes saccades to over- or undershoot the target, which is the eye movement equivalent to limb dysmetria of cerebellar diseases.
Saccades are often directed to novel targets, but more commonly they are made to objects from which information is needed for the execution of a task, for example, to the spoon needed to stir the coffee, or the nail that will be hit with a hammer. This suggests that the saccadic system has swift access to memories of where things are in the surroundings and information about their identities7.
Typically, the examiner tests voluntary saccades that are generated in response to a command. Saccades: both horizontal and vertical, should be assessed for latency, velocity, accuracy, and conjugacy. Dysmetria is a term used to describe inaccuracy of saccades.
There is a hierarchy of testing difficulty: most basic is examining the quick phases of optokinetic nystagmus, then testing of voluntary saccades, and at the other extreme, testing of antisaccades, which are saccades generated in the opposite direction to a suddenly appearing target2.
Loss of quick phases is usually due to a lesion of premotor burst neurons in the brainstem. Early detection is easiest with use of an optokinetic drum, where loss of the quick phases of the OKN may indicate a saccadic gaze palsy9.
The patient should be asked to switch their gaze between two horizontal and two vertical targets. The velocity and accuracy of the saccades should be observed, and whether they are conjugate. In healthy subjects, the target will be reached immediately or will be made by one correctional saccade10.
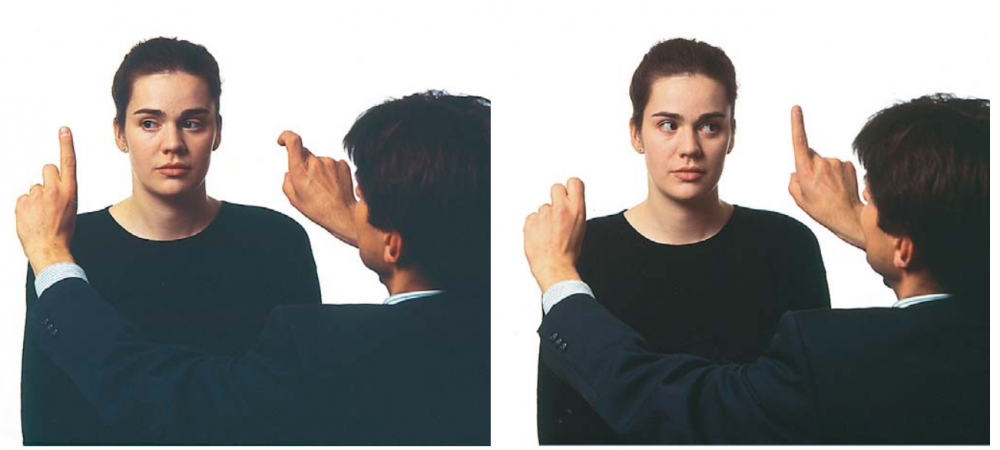
Figure from: Strupp M, Hüfner K, Sandmann R, et al. Central oculomotor disturbances and nystagmus: a window into the brainstem and cerebellum. Dtsch Arztebl Int. 2011;108(12):197-204.
Saccade Latency (saccade initiation):
This test should establish the latency between the command and the generation of a saccade: human saccades typically follow a target jump within 250 ms11.
Latency, or saccadic reaction time, corresponds to the central neural conduction time and relates to conduction in the entire visual-oculomotor pathway12. Delayed initiation of saccades, also called prolonged latency, is seen in oculomotor apraxia associated with Balint's syndrome, and in some neurodegenerative disorders such as Huntington’s disease.
Patients with delayed saccadic initiation often employ head thrusts or eye blinks to generate saccades, and these features may be the sole clinical sign indicating a mild defect in saccadic initiation. Loss of voluntary saccades with preservation of quick phases is characteristic of acquired ocular motor apraxia2. (Note that this term is a misnomer, as the defect is not an apraxia but a disturbance of the initiation of saccades).
Velocity/Speed of saccades8:
The speed of the saccade from the initial to the target position should be assessed.
Saccade speeds are characteristically related to saccade amplitude, but it is virtually impossible to track a saccade at the bedside, since normal saccades are so fast. Impaired accuracy of saccades is usually appreciated by the subsequent corrective saccades needed to bring the eyes to the visual target1.
It is important to examine vertical and horizontal saccades independently, as different disorders selectively affect horizontal and vertical saccades.
Assessment of diagonal saccades (from up and right to down and left, for example) may also be helpful.
Slow saccades can result from central or peripheral lesions (including nuclear and infranuclear lesions).
Peripheral lesions almost always produce slowed saccadic movements that are hypometric. In contrast, slow saccades with normal amplitude are typically due to CNS lesions, especially lesions of the cerebral hemispheres or basal ganglia. Irrespective of the location of a CNS lesion, slowed saccades ultimately result from decreased discharge frequency of excitatory premotor burst neurons (EBN) causing a deficit in phasic innervation (the pulse component) of the saccade. Alternatively, if omnipause neurons (OPN) are damaged, this will slow EBN firing and lead to slow saccades, typically due to damage to the nucleus raphe interpositus, within the PPRF2.
Saccadic slowness confined to the horizontal plane suggests dysfunction of the PPRF in the pons, whereas isolated slowing of vertical saccades indicates a midbrain lesion in which the rostral interstitial medial longitudinal fasciculus (riMLF) is involved, typically due to ischemic or neurodegenerative diseases, especially progressive supranuclear palsy (PSP), or inherited disorders such as Niemann–Pick disease type C6.
Other CNS disorders that cause slow saccades include cerebellar degeneration, Huntington disease, Wilson disease, and Whipple disease, most of which also have prolonged latency at initiation of saccades.
Accuracy of saccades (metrics)8,10:
Accuracy of saccades, and the presence of hypermetric or hypometric saccades should be establised. Saccadic accuracy is expressed as a percentage ratio of the saccade amplitude to the target movement amplitude (gain of the saccade) and is believed to be determined by cerebellar or cerebellar-pathway processing12.
Normal subjects may have a small amount of dysmetria, often with a few degrees of hypometria, especially with relatively large, centrifugally directed saccades: saccades made to target jumps >100 in amplitude often undershoot the target by ≈10% (saccadic hypometria) , and, after a short latency (≈150 ms), are followed by a corrective saccade7. The accuracy of saccadic eye movements can be diɽcult to assess in patients with signiɹcant bilateral loss of vision, especially those with large visual ɹeld defects (eg, homonymous hemianopia and bitemporal hemianopia).
Hypermetric saccades, which can be identified by a corrective saccade back to the object, indicate lesions of the cerebellum (especially the vermis). Patients with Wallenberg’s syndrome make hypermetric saccades toward the side of the lesion and hypometric saccades toward the contralteral side due to a dysfunction of the inferior cerebellar peduncle (conversely, defects of the superior cerebellar peduncle lead to contralateral hypermetric saccades).
Myasthenia gravis may produce faster-than-normal (“lightning-like”) saccades that suddenly stop short of the intended target (reduced saccadic amplitude)
Range of motion and conjugacy of saccades10:
Range of motion should be assessed.
If there is limited range of motion, the next step is to see if such limitations are present with smooth pursuit and vestibular ocular reflexes. The hallmark of a supranuclear brainstem saccadic gaze palsy with impaired range of motion, such as that seen with PSP, is a prominent deficit with saccade testing that may be overcome with vestibular ocular reflexes. Lesions in the midbrain may destroy the EBNs which provide the vertical saccadic drive. By contrast, lesions in the pons may damage EBNs that provide the horizontal saccadic drive11.
Saccadic intrusions or oscillations:
These saccades occur when patients are fixating in the eye primary position, or they may be superimposed during smooth pursuit.
A clinical pearl to heighten sensitivity of detection of saccadic intrusions is to have the patient look in lateral extreme gaze and then back to center, as saccadic intrusions are often provoked by gaze shifts8.
Antisaccades
Antisaccades can be assessed by the examiner holding both hands up and moving a finger on one hand suddenly. The patient is required to look away from the moving finger (ie, to look to the finger that does not move).
Errors on antisaccade tasks are common in lesions of the prefrontal cortex2.
(vv)Saccade.mp4(tt)
From: U-M Kellogg Eye Center in Ann Arbor. Ocular Motility. Retrieved from: http://kellogg.umich.edu/theeyeshaveit/screen/ocular_motility.html
(vv)Saccades 2.mp4(tt)
From: EMBalance Project. Saccades. Retrieved from: https://www.youtube.com/watch?v=D_y56PQvZZA
(vv)Saccades.mp4(tt)
The fast phases of the nystagmus are in the opposite direction to the rotation of the drum