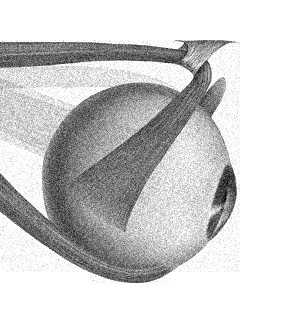
Vergence movements represent an evolutionary adaptation for frontal vision with binocularity. Vergence involves eye movements having to move in opposite directions for simultaneous foveation.
Although vergence disorders are common, they can be challenging to diagnose because convergence depends strongly on patient effort.
These disorders include:
- Convergence insufficiency,
- Convergence spasm
- Divergence insufficiency.
Pathophysiology
Neurons that are important for the convergence reaction lie in the mesencephalic reticular formation and the oculomotor nucleus, explaining why the convergence reaction is disturbed in rostral midbrain lesions and tumors of the pineal region and thalamus. Similarly, abnormalities of vertical gaze are commonly associated with vergence defects.
Examination
Vergence is tested by having the patient look back and forth between a distant and a near target. Looking at a nearby target causes vergence, accommodation and miosis (ie, the convergence reaction).
Note that an inability to converge is not always pathological, as some patients simply converge poorly.
1. Convergence insufficiency
Convergence insufficiency (CI) consists of an exodeviation that is greater at near fixation than at distance fixation. It is a common cause of eye strain, headache, blurred vision, and intermittent diplopia during near-point tasks. Patients with CI have decreased convergence amplitudes and a remote near point of convergence, often greater than 10 cm. This condition often occurs as an isolated finding; in the absence of other neurologic symptoms, further workup is not needed.
Causes:
- Closed head trauma
- Extrapyramidal disorders such as Parkinson disease and PSP
- Lesions of the pretectal area may also be associated with CI; however, such lesions are typically accompanied by other features of dorsal midbrain syndrome (see Parinaud's syndrome). Uncommonly, lesions of the midbrain (within the mesencephalic reticular formation and just dorsal to the CN III nuclei) may cause CI with normal CN III function
Treatment options include monocular occlusion, convergence exercises, prism glasses, and, in rare cases, strabismus surgery.
2. Convergence spasm (spasm of the near reflex)
This consists of intermittent episodes of excess convergence, accommodation, and pupillary constriction.
Causes:
- Isolated spasm of the near reflex is almost always functional.
- When convergence spasm it may be associated with convergence-retraction nystagmus and reduced conjugate upgaze (as in dorsal midbrain syndrome)
- Acquired convergence spasm may also be observed in patients with lesions at the junction of the diencephalon and mesencephalon, thalamus, lower brainstem, and cerebellum, in association with other signs and symptoms related to lesion location (eg, thalamic esotropia due to thalamic hemorrhage, Wernicke's encephalopathy, Arnold-Chiari malformation, multiple sclerosis, midbrain stroke, and phenytoin intoxication).
3. Divergence insufficiency (see also CN 6)
Divergence insuɽciency (DI) is an acquired ocular misalignment defined by an esodeviation that is greater at distance than near fixation, without abduction deficits. This disorder is usually benign and not related to neurologic dysfunction.
In older patients, DI often results from involution of the connective tissue band between the superior rectus and lateral rectus muscles, causing inferior displacement of the lateral rectus muscles (sagging eye syndrome). The malpositioned lateral rectus muscles have reduced abduction force, resulting in DI pattern esotropia.
DI can be confused with bilateral CN VI palsies, incipient unilateral CN VI palsy, or resolving CN VI palsy. Unlike DI, CN VI palsy is associated with slow abduction saccades and abduction deficits. When present as an isolated neurologic finding, DI does not require further workup.
Rarely, DI may be caused by neurological disorders such as:
- Increased intracranial pressure
- Midbrain tumors
- Miller Fisher syndrome
- Head trauma
- Iintracranial hypotension
- ArnoldChiari malformation
- Cerebellar degeneration (often with other signs of these disorders). Treatment options include monocular occlusion, prism glasses, and strabismus surgery.
(vv)Convergence.mp4(tt)