A common adaptation of the HIT is to displace the head laterally first (by 20 degrees), and then rotate the head back to the center position.
The patient's head should be held by the temples, and not the jaw
A positive HIT does not always localize a lesion to the peripheral vestibular system. Other oculomotor signs (see HINTS exam) need review.
The HIT cannot be used to assess VOR function in the presence of a 6th nucleus lesion or paralysis of horizontal extra-ocular muscles.
- The abnormal side is the side identified when the head is thrust towards it, and there is a refixation saccade. In the presence of a peripheral vestibular deficit, the eyes move with the head and a “catch-up” saccade is required to bring gaze back toward the fixation target. The HIT is based on the detection of these “catch up” or refixation saccades.
- The head rotation must be passive (ie, conducted by the examiner) rather than active (ie, deliberate head turn by the patient), since otherwise the patient may make a predictive saccade to correct for an underlying disturbance of the vestibuloocular reflex (VOR)1.
- The HIT should be applied in an unpredictable fashion, that is, the timing, direction, and acceleration are varied in order to keep the patient guessing as to when the next movement may occur1.
- In the patient with an acute vestibular syndrome, there is often spontaneous nystagmus. The refixation saccade of a positive h-HIT must be differentiated from the quick phases of any spontaneous nystagmus.
Background
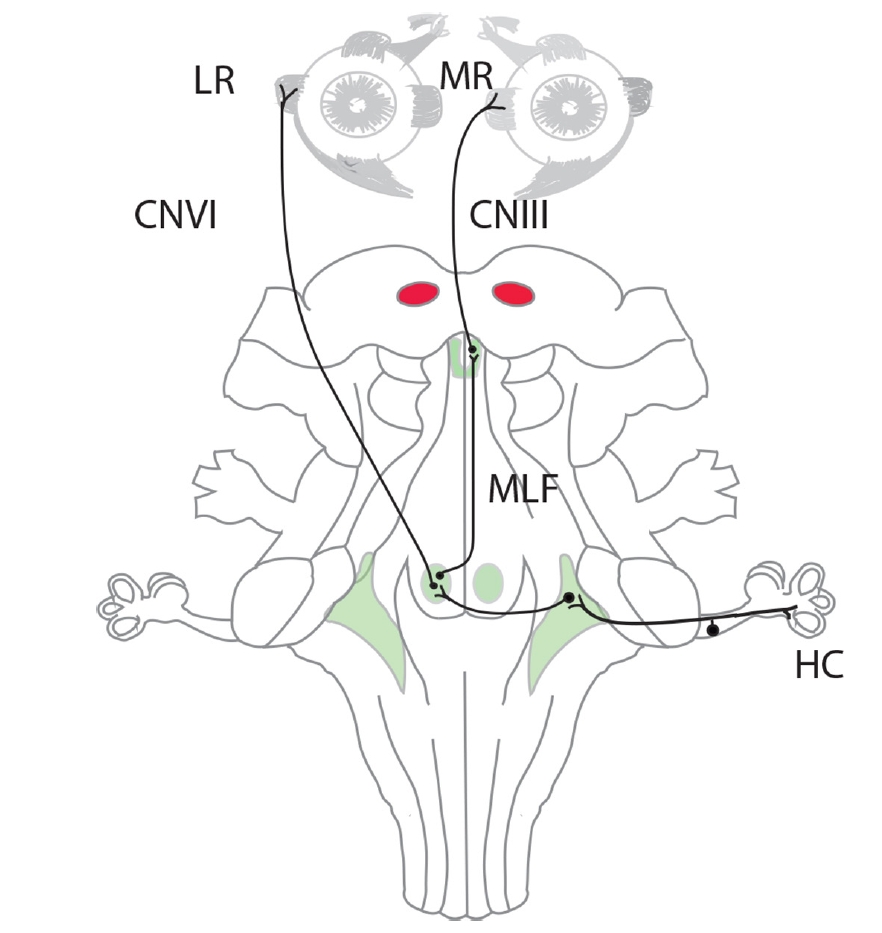
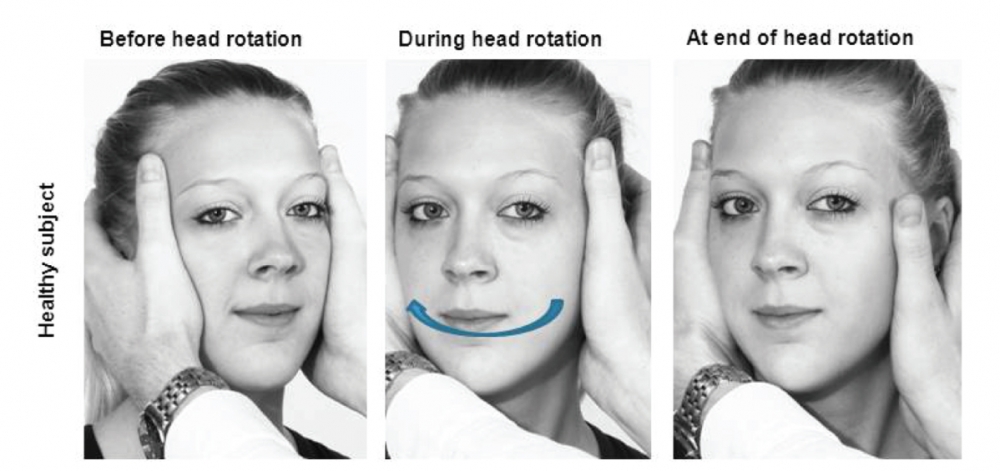
If the peripheral vestibular system is intact and the VOR is functioning normally, the normal VOR response to rapid, passive rotation of the head, while fixating on a central target (eg, the examiner's nose) is an equal and opposite movement of the eyes that keeps gaze relatively stable in space (ie, still looking straight at the target; negative HIT). As one of the fastest brainstem reflexes with a duration of approximately 10 msec, compensating for head rotation is finished before it is perceived by the human eye2. Thus, for the examiner, the subject’s gaze remains stable.
Note that in awake subjects, the ability to maintain gaze on a target as the head is moved slowly from side to side (as opposed to the rapid movement of the HIT) reflects the combined effect of a number of reflexes on the eye (vestibular, visual and cervical). However, if the head is rotated quickly, then visual reflexes will be unable to respond quickly enough, and cervical reflexes are not powerful enough, so that the compensatory counter-rotation of the eyes will be produced almost exclusively by vestibular stimulation, i.e. the VOR, from stimulation mainly of the lateral SCCs, on both sides3.
The normal response is consistent with a VOR gain of 1.0 (ratio of head rotation to eye rotation 1:1). If gain of the VOR is reduced towards the side of the head impulse, retinal slip will trigger a reflexive saccade with a latency of about 100 msec back to the examiner’s nose after the end of the head thrust2. The abnormal response occurs when the head is rapidly rotated toward the side of a vestibular lesion affecting the primary VOR pathway from the vestibular apparatus to the lateral pons. The loss of VOR input results in the subject's inability to maintain fixation during the head rotation, requiring a corrective gaze shift once the head stops moving (positive HIT). This corrective saccade indicates a peripheral vestibular hypofunction on the side towards which the head rotation occurred4.
Vestibular hair cell responses are frequency-specific, much the same as frequency-specific cochlear hair cell responses1. For the VOR, head acceleration is the “frequency” to which the vestibular hair cells are “tuned.” The rotations for the HIT are of low amplitude (10–20Ëš) but of high acceleration2. With too little acceleration (reverting towards the classic “oculocephalic”), the test tends to produce false negatives excepting for those patients with the most severe vestibular failure. With too much acceleration, the test tends to produce false positives, particularly in older patients who may have some asymptomatic (and clinically irrelevant) high-frequency vestibular loss (similar to age-related high-frequency hearing loss).
Horizontal canal receptors ipsilateral to the direction of head movement are preferentially stimulated: the vestibular system stimulates the receptors on the side of the direction of head turning, and actively inhibits the receptors in the contralateral horizontal canal.
The firing rates of vestibular afferents can be driven upward to 300–400 spikes per second, but they can be driven no lower than zero, an inhibitory cutoff. Consequently, stimuli which excite the labyrinth produce a better response than those which inhibit it, a principle known as Ewald’s second law. This difference (between excitation and inhibition) is most profound for strong inputs, such as a high acceleration, high velocity stimulus, as carried out in the HIT. Ewald’s second law results in an asymmetric gain of the VOR (ie, the gain during high acceleration head rotations towards the healthy side is greater than towards the lesioned side)4.
Clinical Correlations
Clinicians with neuro-otological experience have lower HIT sensitivity (ie, are more conservative in rating the HIT as abnormal) and higher specificity (ie, are better at identifying a normal HIT).
Since the VOR gain is not perfect even in healthy subjects, small correcting saccades can often be observed despite intact labyrinths on both sides. In addition, as clinicians tend to compare correcting saccades between the two sides, physiological asymmetries of VOR gains might lead to the incorrect impression of a unilateral deficit. Neuro-otological experts appear to be more tolerant of accepting small correcting saccades as being normal. (If a clinician views every correcting saccade as indicating a pathological HIT, HIT sensitivity increases but specificity decreases4).
Covert Saccades
Overt saccades after head rotation are the telltale sign of vestibular loss, whereas covert saccades during head rotation are imperceptible to the naked eye.
A normal HIT does not rule out vestibular dysfunction: the test is specific, but lacks sensitivity, and consequently, more sensitive adaptations of the test been have developed, such as video HIT.
Assessing other semicircular canals
The standard horizontal-HIT (h-HIT) has also been used to investigate the function of the two vertical semicircular canals (anterior [a-HIT] and posterior [p-HIT]).
Assessing the utricle and saccule
A similar test using a linear head motion (the “head heave” test) has also been developed to interrogate function of the linear-acceleration-detecting otolith organs (utricle and saccule)1.
Indications:
1. Acute vestibular syndrome: to distinguish PICA stroke from vestibular neuritis. Normal HIT rules out PICA stroke, whereas an abnormal HIT may indicate either neuritis or lateral pontine involvement due to AICA involvement. The three-neuron horizontal VOR arc does not pass through the cerebellum or the lateral medulla, the region of supply of the PICA.
2. Chronic vestibular symptoms: detection of residual features after a prior episode of acute vestibular neuritis. An abnormal HIT would sugguest underlying peripheral vestibular problem in most cases.
3. Oscillopsia: diagnosis of bilateral vestibulopathy may be made on basis of abnormal HIT bilaterally.
In a healthy subject, the vestibulo-ocular reflex will keep the eyes on the target.
From: Petersen JA, Straumann D, Weber KP. Clinical diagnosis of bilateral vestibular loss: three simple bedside tests. Ther Adv Neurol Disord. 2013;6(1):41-5
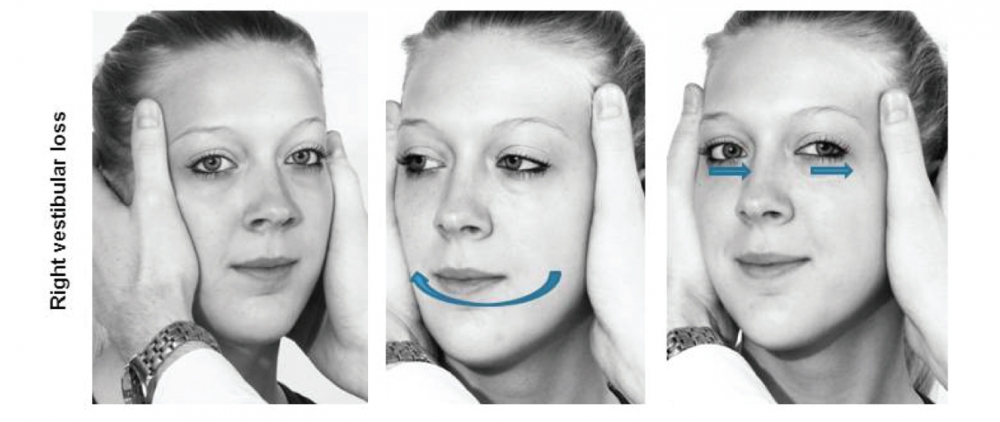
From: Petersen JA, Straumann D, Weber KP. Clinical diagnosis of bilateral vestibular loss: three simple bedside tests. Ther Adv Neurol Disord. 2013;6(1):41-5
(vv)TARNHIT.mp4(tt)
Dieterich M, Tarnutzer AA. Bedside ocular motor testing and vestibular testing. EAN 2020.
(vv)Htt.mp4(tt)
Note the discussion refers to HINTS examination: Head-Impulse, Nystagmus, Test of Skew
(vv)Hit-1.mp4(tt)
(vv)VelocityHIT.mp4(tt)
Halmagyi GM. Clinical Examination of the Vestibular System. J Vestib Res. Teaching Course, 29th Bárány Society Meeting, Lecture 2, June 5, 2016, Seoul, Korea.
From: https://www.youtube.com/watch?v=ehR7SOlBBow
Red: canal activation. Blue: canal inhibition. Green: canal dysfunction. Overt saccades that compensate for deficient canal function are indicated with click sounds.
(vv)HIT schedmatic.mp4(tt)
Acute peripheral vestibulopathy with left-beating, unidirectional nystagmus, which increased on looking in the direction of the fast phase, and with removal of fixation. There is an abnormal HIT to the right, with refixation saccades.
(vv)kattah_video1a_apv_hitabnormal.mp4(tt)
From: Newman-Toker DE, Kattah JC, Alvernia JE, Wang DZ. Normal head impulse test differentiates acute cerebellar strokes from vestibular neuritis. Neurology. 2008;70:2378-2385
Although this patient has a severe vestibular lesion (surgically induced), he has no visually evident catch-up saccades, since he is able to generate the saccade during the head thrust. This would require Video-HIT to detect.
(vv)Covert Sacc.mp4(tt)
Halmagyi GM. Clinical Examination of the Vestibular System. J Vestib Res. Teaching Course, 29th Bárány Society Meeting, Lecture 2, June 5, 2016, Seoul, Korea.
From: https://www.youtube.com/watch?v=ehR7SOlBBow
Demonstrating use of the head heave test, which assesses the translational VOR, the tVOR: a funcion of the utricle and saccule.
(vv)Heave.mp4(tt)
Halmagyi GM. Clinical Examination of the Vestibular System. J Vestib Res. Teaching Course, 29th Bárány Society Meeting, Lecture 2, June 5, 2016, Seoul, Korea.
From: https://www.youtube.com/watch?v=ehR7SOlBBow

