Saccadic pulse dysmetria is a hallmark of disease within the cerebellum and cerebellar-pathways. The dorsal vermis and fastigial nucleus are key cerebellar structures concerned with the control of saccadic accuracy and in the calibration of the size of the saccadic pulse. The cerebellum receives input both from the cortical eye fields (indirectly via pontine nuclei) and the superior colliculus.
Lesions of the dorsal "oculomotor" vermis and the fastigial nucleus typically give rise to inaccurate saccades (dysmetria). These generally take the form of hypermetric or “overshoot saccades” and, less commonly, hypometric saccades.
Lesions in this region can also produce macrosaccadic oscillations.

1. The Fastigial Oculomotor Region (FOR) on each side of the cerebellum facilitates the generation of saccades toward the opposite side (contralateral saccades) and helps with the termination of saccades toward the same side (ipsilateral saccades)1 .
This takes place via projections from the FOR to the omnipause neurons and excitatory/inhibitory burst neurons in the brainstem; the axons arising from the fastigial nuclei decussate within the cerebellum and terminate primarily in the contralateral vestibular or premotor brainstem nuclei2: for example, the right FOR increases its activity before the beginning of leftward saccades and toward the end of rightward saccades.
Impaired function in one FOR may result in:
-Saccade hypermetria toward the same side (as the FOR impairment) (ie saccade contrapulsion)
-Hypometria toward the opposite side (ie saccade ipsipulsion).
Note that a unilateral structural FOR lesion does not occur, since the FOR output crosses immediately and runs through the contralateral FOR before leaving the cerebellum through the superior cerebellar peduncle (Figure 1).
2. The dorsal (oculomotor) vermis OMV behaves in a similar but reciprocal way since it has an inhibitory effect on the FOR.
Therefore, the pattern of saccade dysmetria with lesions in the OMV is the opposite to that with lesions in the FOR:
-Saccade hypometria toward the same side as the lesion
-Hypermetria toward the opposite side of the lesion1.
(vv)Hypermetricsaccade.mp4(tt)
Other functions of the FOR and OMV
- Pursuit
The OMV and its underlying FOR have a similar functional contribution to control of pursuit as for the saccades.
-Lesions of the FOR result in impaired pursuit away from the side of the lesion, but enhances acceleration of ipsilateral pursuit3.
-Lesions of the OMV result in pursuit being impaired toward the same side as the lesion.
The smooth pursuit deficit is predominantly at onset and termination, whereas the vestibulocerebellum/flocculus is more concerned with pursuit during sustained tracking.
- Posture and Balance
Integration of vestibular and proprioceptive information in the rostral fastigial nucleus of the vestibular cerebellum is vital for accurate control of posture and balance self motion perception.
Pathogenesis of Saccadic Hypermetria and Hypometria due to lesions of the FOR and OMV
Cerebellar control of saccades can be understood if one considers the neuroanatomical circuitry:
The oculomotor vermis receives information about performance during saccades and adjusts its inhibition upon the FOR to assure the saccade arrives on target2. The oculomotor vermis is also important for saccade adaptation to occur, and the plasticity for this motor learning occurs at the level of its Purkinje cells, based on an error signal which arises in the superior colliculus5.
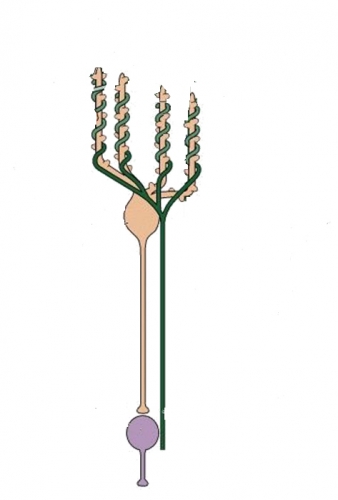
The paramedian pontine reticular formation (PPRF) contains excitatory burst neurons (EBN), and caudal to it is a region of the medullary reticular formation (MRF) which contains inhibitory burst neurons (IBN), which project to the contralateral abducens nucleus, as shown in Figure 1 below:

Firing of both EBMs and IBMs on the right side, for instance, provide an excitatory pulse to the right abducens nucleus with a resultant saccade to the right, as well as concurrent inhibition of the antagonist muscles, the left lateral rectus and the right medial rectus via the medial longitudinal fasciculus.
Both the pontine and medullary reticular formations (PPRF and MRF) receive excitatory projections from the contralateral fastigial nucleus, via the uncinate fasciculus. This pathway crosses the midline and bends around the superior cerebellar peduncle on the way to the brainstem.
Saccade accuracy and Fastigial Nucleus (FOR) Lesions
A lesion of the left fastigial nucleus, or an equivalent lesion of the underlying deep cerebellar white matter (hook bundle) in the region of the right superior cerebellar peduncle, would result in decreased excitation of EBNs and IBNs on the right. This would lead to hypometria of rightward saccades.
The fastigial nucleus is also concerned with decelerating ipsilateral saccades. Similarly to the antagonist burst of an agonist-antagonist muscle activation, cells in the left fastigial nucleus will fire prior to the end of leftward saccades, and by exciting IBNs on the right, will cause inhibition of abducens motor neurons on the left side. A failure to generate this inhibition would result in a prolongation of the pulse applied to the left abducens motor neurons and consequently hypermetric saccades.
Contrapulsion is the situation found in a hook bundle lesion, where hypermetric saccades are seen, away from the side of the lesion, associated with hypometric sacades towards the side of the lesion6.
Lesions of the Oculomotor Vermis
A lesion of the OMV would stop cerebellar cortical inhibition of the deep cerebellar nuclei, including the FOR, resulting in overactivity of the FOR.
Consequently, there will be contralateral hypermetria of saccades: contrapulsion.
Lesions of the Inferior Cerebellar Peduncle (Wallenberg syndrome) (see video of ipsipulsion)
Fastigial neurons receive inhibitory projections from Purkinje cells of the ipsilateral cerebellar vermis. The Purkinje cells receive climbing fibre input from the contralateral inferior olive via the inferior cerebellar peduncle, as well as mossy fibre input via the middle cerebellar peduncle. When a climbing fibre excites a Purkinje cell, there is a refractory period with diminished Purkinje cell inhibitory activity on fastigial neurons. A lesion of the inferior cerebellar peduncle therefore will cause loss of climbing fibre input, and fewer Purkinje cell refractory periods. This results in a net increase in Purkinje cell inhibition of fastigial neurons, and functional inhibition of the FOR unilaterally.
For example, a left sided Wallenberg syndrome will cause increased inhibition of the left fastigial nucleus (FOR), and result in:
-ipsipulsion with hypermetric saccades to the left, towards the side of the lesion.
-hypometric saccades to the right.
Ipsipulsion (to the right) under closed lids, and lateropulsion (to the right) of vertical saccades. Probably right sided medullary lesion due to demyelination..
(vv)SaccH.mp4(tt)
From: Gold D.Saccadic hypermetria and ipsipulsion (behind closed eyelids and with vertical saccades. Video. [Neuro-Ophthalmology Virtual Education Library: NOVEL Web Site]. 2018. Available at: https://collections.lib.utah.edu/ark:/87278/s64r24wd
(vv)TARNHYPO.mp4(tt)