Similarly to trigeminal neuralgia, neurovascular compression of the 8th cranial nerve may give rise to intermittent symptoms due to ephaptic cross-talk between partly demyelinized axons. The likely site of the lesion is the central myelin (oligodendrocytes), proximal to the transition zone of the nerve. This corresponds to the first 12 mm immediately after the nerve exits from the brainstem1. Paroxysmal stimulation of the brainstem, as occurs in multiple sclerosis, may give rise to similar complaints2.
The duration of attacks is typically short, lasting from seconds up to a few minutes; the number of attacks is variable, from 30 a day to a few annually1. The disorder is typically chronic, of more than three months' duration.
The main symptoms and signs are short attacks of oscillopsia and vertigo with nystagmus, and postural imbalance2. The attacks consist of rotatory (occasionally postural) vertigo with or without auditory symptoms (tinnitus and hearing impairment). If a patient is examined during an attack, a horizontal and torsional nystagmus which beats toward the affected ear may be seen.
If the attacks occur while standing or walking patients usually experience unsteadiness1.
An attack may be provoked by prolonged hyperventilation3, since hyperventilation leads to alkalosis and changes in the transmembraneous potential of cells bringing about increased excitability, and may result in transient nystagmus in vestibular paroxysmia2.
In over 95% of cases high-resolution MRI of the brainstem, specifically a CISS (Constructive Interference in Steady State) sequence, demonstrates vessel–nerve contact at the exit point of the eighth cranial nerve from the brainstem3. Of importance however, is that close contact between AICA and the 8th cranial nerve is seen in up to 40% of normal subjects4.
Diagnostic criteria2
A) At least ten attacks of spontaneous spinning or non-spinning vertigo
B) Duration less than 1 minute
C) Stereotyped phenomenology in a particular patient
D) Response to treatment with carbamazepine/ oxcarbazepine
a) High-resolution MRI of the cerebellopontine angle depicting the contact between the vestibulocochlear nerve and the anterior
inferior cerebellar artery (CISS sequence)
b) Time-of-flight (TOF) sequence for improved visualization of vessels; AICA, anterior inferior cerebellar artery
c) The vessel–nerve contact visualized intraoperatively
d) Compression of the nerve after removal of the artery (circle)
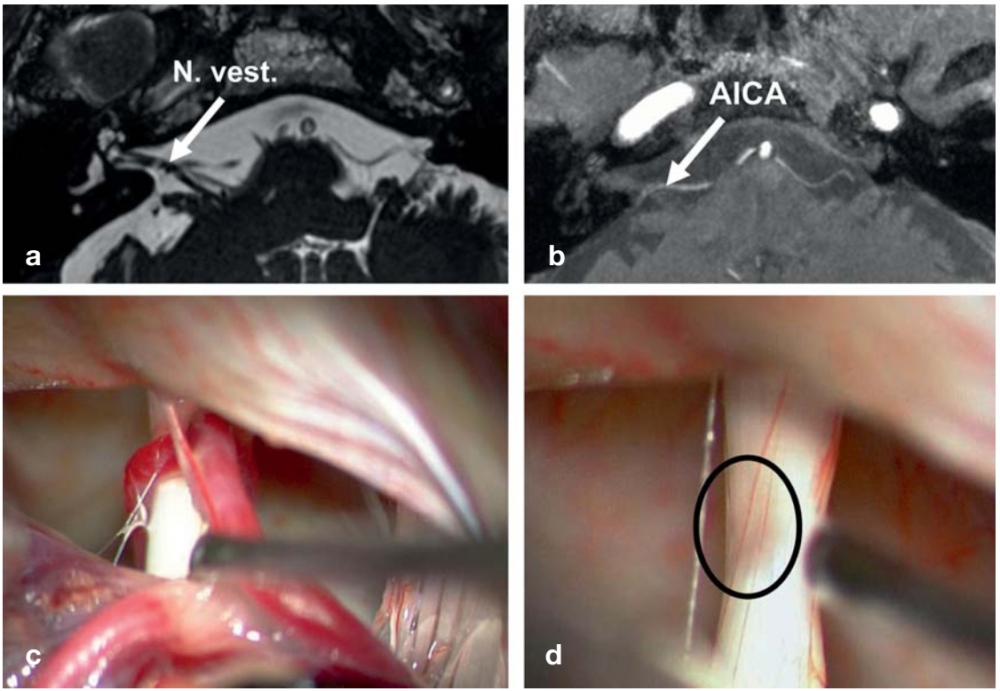
From: Strupp M, von Stuckrad-Barre S, Brandt T, Tonn JC. Teaching neuroimages: Compression of the eighth cranial nerve causes vestibular paroxysmia. Neurology. 2013;80(7):e77.
(vv)Parox.mp4(tt)
From: Strupp M. How to take a patient history: Video Quiz. EAN 2020
Treatment
As with trigeminal neuraglia, carbamazepine or oxcarbazepine may be of benefit3. If medical therapy is ineffective, nerve compression may be indicated.
Additionally, lacosamide may be of benefit (dose 100-400 mg daily)5.

