- Esodeviations (esotropia and esophoria) occur with impaired abduction of one or both eyes and are defined by one eye deviated medially (toward the nose) relative to the other eye.
- Exodeviations (exotropia and exophoria) occur with impaired adduction of one or both eyes and are defined by one eye deviated laterally (toward the ear) relative to the other eye.
- Hyperdeviations (hypertropia and hyperphoria) occur with impaired depression of one eye and are defined by one eye deviated higher relative to the other eye.
When eye misalignment is to the same degree in all directions of gaze, it is termed comitant: These misalignments are due to disturbances of vergence, and to a breakdown of the brains fusional ability.
When eye misalignment is different in eccentric positions of gaze, it is termed incomitant. These misalignments are due to:
- Internuclear ophthalmoplegia
- Skew deviation
- Oculomotor nerve palsyies
- Disorders of neuromuscular transmission
- Disorders of orbital tissue, Including the extraocular muscles
Differential diagnosis includes: week lateral rectus muscle, tight medial rectus muscle, orbital mass, impaired NMJ transmission, and sixth nerve palsy
(vv)Incom.mp4(tt)
From: Trobe, J https://collections.lib.utah.edu/ark:/87278/s6r272pg
Gross ocular palsies are easy to recognize, however, features on history will often be helpful:
Direction of diplopia:
Diplopia should be assessed as being horizontal, vertical, or oblique, and if it is worse in a particular direction of gaze; and if it is worse at distance or near. Diplopia worse in a particular direction of gaze suggests that ocular motility in that direction is impaired.
- Horizontal diplopia is usually caused by impaired abduction or adduction of an eye
- Vertical diplopia results from impaired elevation or depression
- Diplopia that is vertical and torsional (with the lower image tilted) suggests involvement of the superior oblique muscle, while pure vertical diplopia is more likely to reflect brainstem or cerebellar pathology1.
- Diplopia that is oblique/diagonal, reflecting dysfunction of both vertical and horizontal muscles, suggests dysfunction of the oculomotor nerve1.
Diplopia at distance and at near:
- Diplopia worse at distance usually accompanies impaired abduction or divergence of the eyes (typically a 6th nerve palsy)
- Diplopia worse at near accompanies is seen with adduction or convergence (typically a 3rd nerve palsy); may be associated with difficulty reading.
- Diplopia worse when going down stairs or escalators, or stepping onto a pavement suggests a 4th nerve palsy1.
For example, if a patient describes binocular, horizontal diplopia that is worse on right gaze and worse at distance, this is highly suggestive of impaired abduction of the right eye2.
An alternate cover test in the 6 cardinal positions of gaze is extremely helpful:
- A subtle sixth nerve palsy will manifest as an increasing esophoria/tropia as the involved eye is abducted (that is, on gaze to the side of the nerve palsy) (see Video 1 below).
- A subtle medial rectus palsy will be indicated by an increasing exophoria/tropia as that eye is adducted. A further example would be, in a patient with left INO (failure of left eye to adduct), with alternate cover and cover-uncover testing, there would be an exodeviation that is maximal on right gaze due to an adduction deficit of the left eye3.
- A subtle elevation deficit manifests as a hypophoria/tropia on upgaze, and a subtle depression deficit manifests as a hyperphoria/tropia on downgaze.
In a third nerve palsy, in addition to the exophoria/tropia on adduction, there will be a reversing hypertropia/phoria because the eye has both weak elevation and weak depression. The involved eye is hypotropic on upgaze and hypertropic on downgaze.
Although hypodeviations occur with impaired elevation of one eye, by convention, this is generally described as a hyperdeviation in the opposite eye (eg, if the right eye does not fully elevate, this is functionally a right hypotropia; however, it is more commonly described as a left hypertropia).
70-year-old woman with hypertension and diabetes who presented with horizontal diplopia for several weeks, worse with right gaze. There was a very subtle abduction paresis on the right. MRI showed a small subacute stroke involving the right 6th nerve fascicle within the pons.
-
The video shows esodeviation seen with alternate cover testing.
(Not shown, is that with alternate cover testing there was a very subtle esophoria in primary gaze at distance; with cover-uncover testing, there was a small esotropia in right gaze.)
(vv)6CNcover.mp4(tt)
(vv)IncomEso.mp4(tt)
From: Trobe, J https://collections.lib.utah.edu/ark:/87278/s6mwas78
See also: 6th nerve palsy
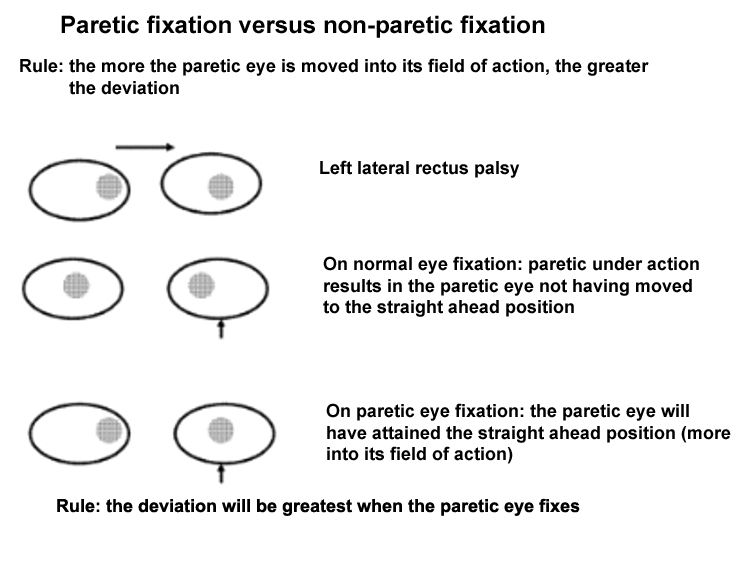
In a recent palsy, when the eye with the weak muscle is fixing, a greater than normal innervation will be needed for the weak eye to get to the primary position, and therefore its yoke muscle in the normal eye will be overactive.
However, if the normal eye is fixing, the eye with the paretic muscle will be deviated because of a paretic underaction.
Yoke overaction is greater than paretic underaction. Therefore, the deviation observed will be greatest when the paretic eye is fixating (termed secondary deviation), and the deviation will be less when the normal eye is fixating (termed primary deviation).
(In long-standing palsies, the deviation will be the same regardless of the eye which is fixating, since the difference between the paretic eye fixation and normal eye fixation tends to disappear, a process which is termed spread of comitancy.)