Epley Manoeuvre Semont Manoeuvre
It is reasonable for neurologists to concentrate on liberation manoeuvres for the posterior and horizontal semicircular canals, since the anterior semicircular canal is not affected commonly.
Positional testing involves the provocation of vertigo and nystagmus, and different manoeuvres test different semicircular canals: a canal-specific response is diagnosed when a rotation of the head in the plane of a semicircular canal evokes positional nystagmus of maximal intensity (in terms of slow phase velocity).
When the head is rotated 45 degrees to the left and rapidly pitched backwards (Dix-Hallpike manoeuvre), the otoconia move along the left posterior canal to lie midway along the duct. The resultant plunger effect or negative pressure causes ampullofugal movement of the cupula and briefly excites the posterior canal afferents1. As a rule (and in contrast to central positional nystagmus), positional nystagmus in BPPV always beats in the plane of the affected canal and in the expected direction for canal excitation.
A supine roll test to assess for lateral semicircular canal BPPV should be performed if the patient has a history compatible with BPPV and the Dix-Hallpike test exhibits horizontal or no nystagmus.
Otoconia shown with patient sitting up (A), with head turned 45 degrees to the right (B), and in the head hanging position (C). mage of the semicircular canals viewed from the patient's right side.

From: Huh YE, Kim JS. Bedside evaluation of dizzy patients. J Clin Neurol. 2013;9(4):203-213. doi:10.3988/jcn.2013.9.4.203
BPPV of the posterior semicircular canal.
Positioning the patient in a head-hanging posture, with the head turned towards the involved side, may sometimes induce nystagmus and vertigo.
As the patient is being moved, they will correctly perceive head rotation. When the head comes to rest in its new orientation, there is normally no further nystagmus or sense of movement. In the patient with canalithiasis (particles in the duct of the canal), a second excitation occurs as the debris ‘gravitates’ to a new lowest point. This induces a response by the canal which is indistinguishable from that caused by actual rotation of the head in space—there is the same nystagmus and associated perception of rotation, now termed vertigo, which persists for as long as the particles are in motion1.
Noting that all of the features of typical nystagmus provoked by changes in head position in patients with BPPV may be explained by canalithiasis2, the charasteristics of the nystagmus are:
(a) Starts after a short latency (5-20 seconds) (not immediately). (A few beats of nystagmus as the head reaches its final head-hanging destination are normal, unless the head has completely stopped moving).
(b) Dampens after 5-60 seconds. The duration of nystagmus corresponds with the time needed for particles to come to rest in a new dependent location.
(c) May reappear on arising from the Dix-Hallpike position. In this event, it reverses direction: opposite direction to that observed in the head-hanging position: returning the patient from the head-hanging position to an upright position causes reverse flow of otoconia (ampullopetally) and torsional downbeat nystagmus with torsion toward the unaffected ear1.
(d) Fatigues on repeated trials. Repeating the postural testing may induce further episodes, but they usually become progressively less severe with repetitive testing. Assessing fatigueability is not recommended!
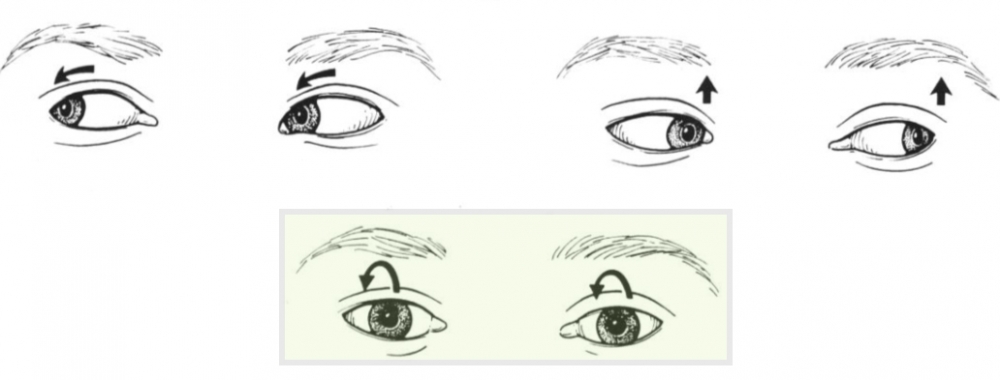
(e) Direction: vertical and torsional components that move the eyes in a plane parallel to that of the posterior semicircular canal being stimulated. The typical nystagmus (best seen with Frenzel’s glasses) beats in the direction of the undermost ear The rotatory-linear nystagmus reflects ampullofugal stimulation of the posterior semicircular canal with activation of the ipsilateral superior oblique and contralateral inferior rectus eye muscles3. The eye ipsilateral to the affected (down) ear has the more pronounced extorsional nystagmus, with the upper pole of the eye beating toward the ground. The contralateral eye is more upbeating1.
(Expressed in space-fixed coordinates, upbeat nystagmus in the head-hanging position (towards the eyebrow and uppper eyelid) is geotropic, that is, directed toward the earth, and downbeat nystagmus is apogeotropic).
Nystagmus direction is dependent on direction of gaze:
–Torsional (uppermost pole beating to lower shoulder/towards the upper eyelid) when looking towards the lowermost precipitating ear.
–Vertical upbeat nystagmus when looking away from lowermost precipitating ear: beats towards the forehead.
- When posturally-induced nystagmus does not have these features, other diseases of the CNS, in particular those involving the posterior fossa, must be considered. For example, a positional nystagmus beating downwards, with or without a torsional component, may be central (unmasked cerebellar downbeat nystagmus) or due to contralateral anterior canalolithiasis.
- Nystagmus fading away within one minute indicates a canalolithiasis; if nystagmus persists, cupulolithiasis is present.
- Patients with a history compatible with BPPV (ie, repeated episodes of vertigo produced by changes in head position relative to gravity) who do not appear to have posterior semicircular canal BPPV by Dix-Hallpike positioning should be tested for lateral/horizontal semicircular canal BPPV3.
Vestibulospinal Respones
When attacks of BPPV occur when standing, after a short latency patients develop large amplitude swaying predominantly in the fore-aft direction. The amount of instability decreases gradually within 30 seconds as the sensation of vertgo diminishes.
Patients in the acute phase of BPPV may also complain of unsteadiness of gait and balance, which they describe as walking on pillows. These symptoms can be classified as otolithic vertigo4.
In this subject with right posterior semicircular canal BPPV due to canalolithiasis, after a 2 second latency in the right Dix-Hallpike position, a burst of upbeat and torsional nystagmus with the upper pole of the eye beating toward the right ear is elicited and lasts for 12 seconds.
(vv)BaranyPosteriorcanalbppv.mp4(tt)
From: Committee for the International Classification of Vestibular Disorders of the Barany Society.2.3.1.1.1. Posterior semicircular canal benign paroxysmal positional nystagmus.
Retrieved from http://www.jvr-web.org/images/2.3.1.1.1.-Posterior-canal-BPPV.m4v
Patient shown initially with head turned to the left (normal side). Subsequently, turns the head is turned to the right side, and nystagmus develops.
(vv)PostC.mp4(tt)
From: Halmagyi GM. Clinical Examination of the Vestibular System. J Vestib Res. Teaching Course, 29th Bárány Society Meeting, Lecture 2, June 5, 2016, Seoul, Korea.
From: https://www.youtube.com/watch?v=ehR7SOlBBow
The rationale for every liberation manoeuvre is to remove detritus out of the affected semicircular canal, thereby taking into account that one of the two exits of every semicircular canal is blocked by a cupula.
The modified Epley manoeuvre is a manual treatment for posterior canal-BPPV (p-BPPV) that involves rotating the head in such a way so as to free the debris from the posterior semicircular canal. It was the first such manoeuvre developed, and is the only therapy recommended with strong evidence by an evidence-based guideline for treatment of p-BPPV. The success rate of repeated performance of the Sémont liberatory manoeuvre or the Epley repositioning manoeuvre is over 95% in p-BPPV.
- Patients with severe nausea should be given antivertigo drugs 30 minutes before the manoeuvre.
- Available evidence suggests that vibration or percussion of the mastoid is unnecessary5.
- The success of a liberation manoeuvre may be confirmed by repetition of the corresponding provocation manoeuvre, provided the patient is not too nauseous. If positional vertigo and nystagmus persist, the liberation manoeuvre should be repeated during the same or at a follow-up visit. If the liberation manoeuvres remain unsuccessful over a period of 2 weeks, consider further investigations, such as cranial MRI, in order to exclude central causes of positional vertigo.
- Bilateral BPPV is difficult to treat during a single visit, because a liberation manoeuvre on one side may undo the previous liberation manoeuvre on the other side. Suggested therefore to treat one side only during the first visit, and the other side one day later.
In some patients, after careful instruction including practical demonstration and the provision of diagrams, they are able to perform the liberatory manoeuvre at home (frequency and duration: three times in the morning, three times in the afternoon, and three times in the evening, usually for three days). The most important thing is to ensure correct positioning of the head.
After a succesful manoeuvre the debris will fall into the utricle: this may result in otolith stimulation with postural imbalance for a few weeks. Patients should be encouraged to engage in all normal activities as far as they are able despite this postural imbalance.
- Patients may be able to report that they become symptomatic when they turn to one side: the affected side is that which results in symptoms when the patient turns to that side.
- Alternatively, performing a Dix-Hallpike test should identify the affected ear (the patient can be instructed to do this themselves before the visit).
Note Steps 1 and 2 are the same as the Dix-Hallpike manoeuvre; in Steps 3 and 4 the physician turns the patient through 90 degrees twice.

Redrawn from: Fife TD, Iverson DJ, Lempert T, et al. Practice parameter: therapies for benign paroxysmal positional vertigo (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2008;70(22):2067-2074. doi:10.1212/01.wnl.0000313378.77444.ac
REPEAT:
On the basis of wishing to ensure that the treatment has been succesful, (or the converse), one may wish to repeat the manouevure; this is controversial, and patients may find it unpleasant:
- After waiting 30 seconds or so, repeat the whole manoeuvre.
- If there is no paroxysmal nystagmus or symptom during Dix Hallpike positioning (Steps 1, 2), this suggests that the repositioning manoeuvre has been successful.
- Important to complete the final Epley cycle (Steps 3-5), in case debris fell back into the posterior canal during the second Dix-Hallpike positioning.
Adverse Events
10% chance of nausea, vomiting, and syncope.
p-BPPV may be converted to h-BPPV, or a-BPPV.
Immediately after a successful liberation manoeuvre, patients may sometimes experience a falling sensation, which is possibly due to detritus falling on the utricular membrane.Imbalance for hours or even days after a successful liberation manoeuvre is common.
Post-treatment instructions
Despite initial caution, staying upright for 1-2 days appears to be unnecessary6.
After a successful liberation manoeuvre, the patient should avoid high-acceleration head movements (eg. jogging, jumping) and head positions below the horizontal (eg, visiting the dentist) for 3 days. This minimizes the risk of a BPPV recurrence.
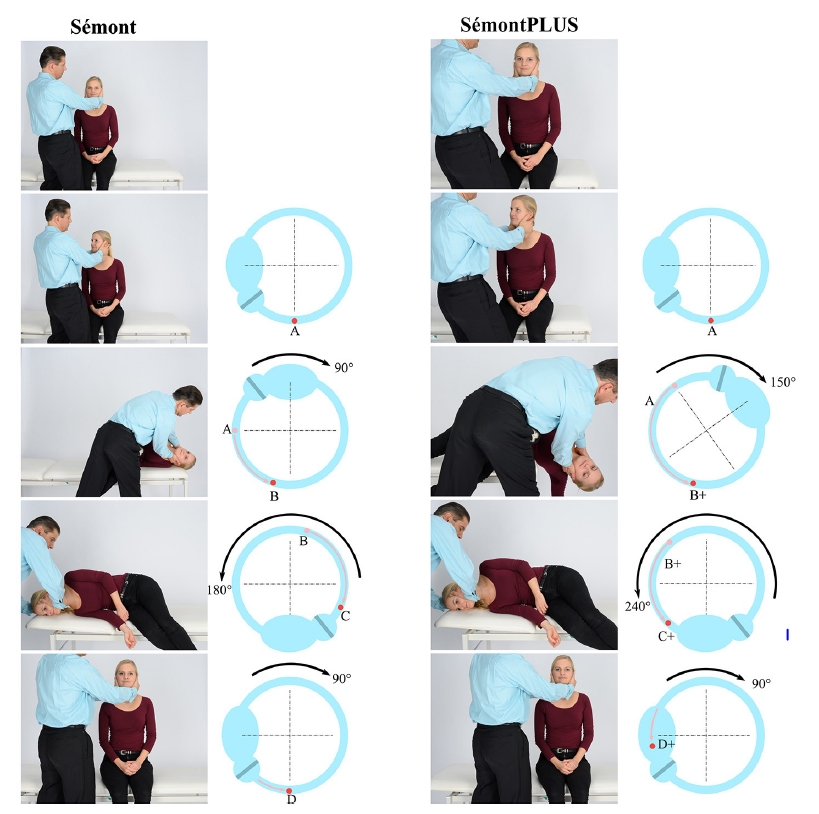
Semont Manoeuvre7
The examiner stands in front of the patient, who is seated on the side of the examining couch: the head is turned 45° away from the affected ear. Note that is opposite to the direction of head rotation used in the Dix-Hallpike manoeuvre.
Note also that this direction of head rotation is opposite to the subsequent direction of movement of the body. For example. the head is turned 45° to the right and the body is then moved to the left side.
For right BPPV the body is shifted to the right:
1. The body is moved rapidly from the sitting position to a horizontal or head hanging position and maintained in that position for 60 seconds: the side-lying position.
2. The body is then moved towards the unaffected side in a 180° cartwheel motion \and maintained in that position for 60 seconds. The head is maintained in the same position relative to the shoulders, that is, the face is pressed into the examining couch.
Note that with liberatory manoeuvres, the further the head is turned towards the unaffected side during the movement of the body toward the unaffected side, the higher the efficacy of the liberatory maneuver.
3. The patient is then brought to an upright seated position and maintains that position for 60 seconds.
The expected response to the liberatory maneuver is another episode of intense vertigo and paroxysmal nystagmus with the same direction of rotation as in the provoking Dix–Hallpike position, which is due to the movement of debris in the ampullofugal direction, towards the utricule. This is called liberatory nystagmus and is therefore a good prognostic sign; its absence is almost always a sign that the maneuver has been unsuccessful7.
Fifteen to sixty minutes after the first therapeutic maneuver, a second diagnostic maneuver may be performed to check the effect of the first maneuver, i.e., whether positional vertigo and/or positional nystagmus can still be induced.
The Semont Plus refers to overerextension of the head by 600 below earth horizontal during the movement of the patient toward the affected side. It reportedly is associated with a more recovery following the liberatory manoeuvre, as compared to the Semont manoeuvre; note that this study requested the patients to carry out the manoeuvre nine times a day (3 manoeuvres in the morning, midday and evening) after the initial manoeuvre carried out by the physician8.
In both manoeuvres (Semont and Semont plus), a single manoeuvre may only be succesful half the time and repeated manoeuvres may be needed (including self-guided manoeuvres).
This also predicts that more otoconia should then move beyond the vertex of the canal when the patient is subsequently moved toward the unaffected side.
(vv)EPLEYSCC.mp4(tt)
From: Straumann D. How to diagnose and treat benign paroxysmal positional vertigo. EAN 2020
(vv)Epley.mp4(tt)
From: Straumann D. How to diagnose and treat benign paroxysmal positional vertigo. EAN 2020
(vv)Semont Plus.mp4(tt)
From: Strupp M, Goldschagg N, Vinck AS, Bayer O, Vandenbroeck S, Salerni L, Hennig A, Obrist D, Mandalà M. BPPV: Comparison of the SémontPLUS With the Sémont Maneuver: A Prospective Randomized Trial. Front Neurol. 2021 Apr 14;12:652573.

