Blepharospasm is a dystonia of the facial musculature that ranges in severity from an increased blink rate to disabling contractions with pain and visual dysfunction.
Blepharospasm is characterized by excessive contraction of the orbicularis oculi muscles, and patients often may attempt eyebrow elevation to overcome the problem; similarly, patients may commonly attempt to prise their lids apart with their fingers (as seen in the video). Increased blinking is believed to represent a forme fruste of blepharospasm.
Diagnosis is based on clinical recognition.
Exacerbating and alleviating factors, the presence of sensory tricks, and dystonia elsewhere should be evaluated.
Blepharospasm is often improved by concentration or by tasks requiring the subject's attention.
Brain imaging is rarely needed; blood tests are unrevealing.
Differential diagnosis:
- Apraxia of eyelid opening, common in Parkinson’s disease and PSP, which is characterized by failure to activate the levator palpebrae muscle on attempted eye opening (note that these conditions may be also have blepharospasm associated)
- Meige’s syndrome or segmental cranial dystonia is the association of blepharospasm with oromandibular and sometimes cervical or laryngeal dystonia.
- Ptosis: eyelid closure without muscle spasm
- Tics: typically it would be anticipated that a premonitory urge and ability to voluntarily suppress the movement might be present.

Anatomy
The orbicularis oculi muscle lies in a plane just deep to the subcutaneous tissue; the skin of the eyelids is the thinnest skin in the body and contains very little subcutaneous fat. Thus, the orbicularis oculi muscle may lie just 1 mm below the surface of the skin. The muscle is divided into orbital and palpebral parts:
- Orbital portion forms a wide circle around the orbital rims and interdigitates with other facial muscles. It is under voluntary control and is responsible for tight closure of the eyelids.
- Palpebral part involuntarily and gently closes the eye during blinking and sleep and is further divided into:
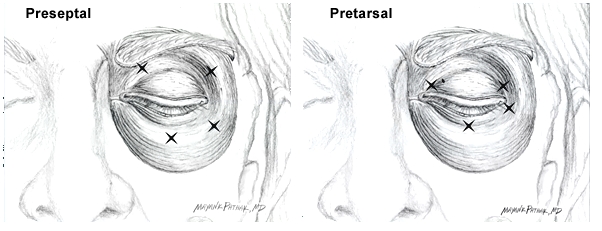
- Preseptal portion that overlies the orbital septum
- Pretarsal portion that extends between the medial and lateral canthi anterior to the tarsus.
From: Truong D, Dressler D, Hallett M, Zachary C, editors. Manual of Botulinum Toxin Therapy [Internet]. Cambridge University Press; 2014
Treatment
Artificial tears are recommended for eye dryness, but do not improve spasm.
Surgical myotomy or myectomy produces relief in over 80% of patients, but symptoms may recur. Surgery may also incur complications including bruising, numbness, eyebrow/eyelash loss, and skin loss requiring grafting and disfiguration; therefore, it is largely reserved for patients with severe symptoms that are not controlled with toxin injections.
It is recommended to avoid injection of botulinum toxin in the following sites:
- In the centre of the upper eyelid to avoid diffusion to levator palpebrae with subsequent ptosis
- The inferomedial region to avoid interference with the lacrimal drainage apparatus
Commonly a combination of the pretarsal and preseptal injections is useful; pretarsal injections may have a longer duration of benefit and fewer side effects, such as ptosis. However, preseptal and/or orbital injections can be included if those areas appear especially active.
- Pretarsal: over lateral and medial aspect of upper lid
- Preseptal: over the lateral margin of the orbit (two sites), and the lower eyelid.
Dose: typically 2-2.5 units Botulinum: total of 5 injections per eye (12. 5 u); total 25 units for both eyes.
A survey of oculoplastic surgeons found a mean starting dose of 22.5 9.5 U onaBoNT-A per eye.35 The mean maximal dose to induce a stable response among their patients was 50 U per eye
Common side effects include ptosis, entropion, bruising, tearing, dry eyes, lagophthalmos, keratitis, and diplopia. All are rarely severe and are reversible. Longitudinal studies have shown no worsening or other adverse effects with repeated use over more than 20 years.


