From: Iankova V, Respondek G, Saranza G, Painous C, Cámara A, Compta Y, Aiba I, Balint B, Giagkou N, Josephs KA, Otsuki M, Golbe LI, Bhatia KP, Stamelou M, Lang AE, Höglinger GU; Movement Disorder Society-endorsed PSP Study Group. Video-tutorial for the Movement Disorder Society criteria for progressive supranuclear palsy. Parkinsonism Relat Disord. 2020 Sep;78:200-203. doi: 10.1016/j.parkreldis.2020.06.030. Epub 2020 Sep 22. PMID: 32988736.
Levels of
|
FUNCTIONAL DOMAIN
|
|||
OCULAR MOTOR DYSFUNCTION |
POSTURAL INSTABILITY |
AKINESIA |
COGNITIVE DYSFUNCTION |
|
Level 1 |
O1: Vertical supranuclear gaze palsy |
P1: Repeated unprovoked falls within 3 years |
A1: Progressive gait freezing within 3 years |
C1: |
Level 2 |
O2: Slow velocity of vertical saccades |
P2: Tendency to fall on the pull-test within 3 years |
|
C2: Frontal cognitive/behavioural presentation |
Level 3 |
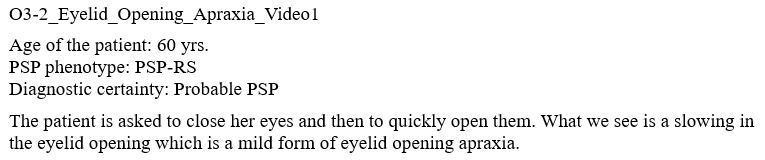
O3: Frequent macro square wave jerks or "eyelid opening apraxia" |
P3: More than two steps backwards on the pull-test within 3 years |
A3: Parkinsonism, with tremor and/or asymmetric and/or levodopa responsive |
|
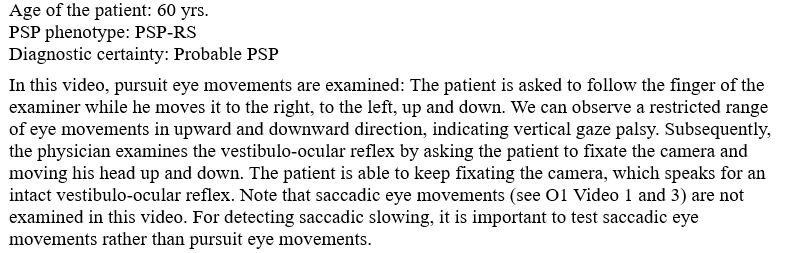
OCULAR MOTOR DYSFUNCTION
DEFINITION: A clear limitation of the range of voluntary gaze in the vertical more than in the horizontal plane,affecting both up- and downgaze, more than expected for age, which is overcome by activationwith the vestibulo-ocular reflex; at later stages, the vestibulo-ocular reflex may be lost, or the maneuver prevented by nuchal rigidity.

(vv)1S20s1353802020302078mmc2-1.mp4(tt)
(vv)VerticalSNGP.mp4(tt)
(vv)1-s2.0-S1353802020302078-mmc3.mp4(tt)

(vv)1-s2.0-S1353802020302078-mmc4.mp4(tt)
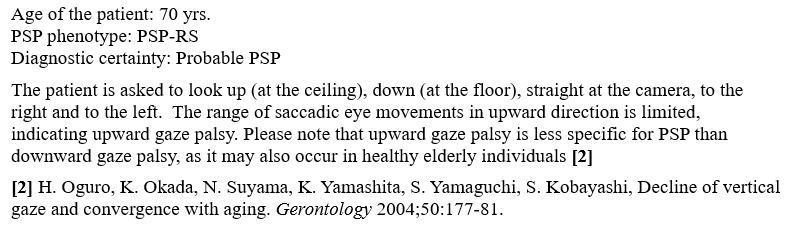
DEFINITION: Decreased velocity of vertical greater than horizontal saccadic eye movements; this may be established by quantitative measurements of saccades, such as infrared oculography, or by bedside testing; gaze should be assessed by command ("look at the flicking finger") rather than by pursuit ("follow my finger"), with a target greater than 20° from the position of primary gaze; to be diagnostic, saccadic movements are slow enough for the examiner to see their movement, rather than just initial and final eye positions as in normal subjects; a delay in saccadic initiation is not considered slowing; findings are supported by slowed or absent fast components of vertical optokinetic nystagmus (i.e., only the slow following component may be retained).

(vv)SlowVerticalSaccades1.mp4(tt)
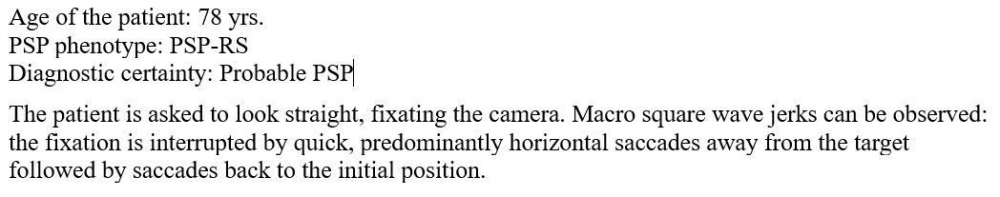
DEFINITION: Macro square wave jerks are rapid involuntary saccadic intrusions during fixation, displacing the eye horizontally from the primary position, and returning it to the target after 200-300 ms; most square wave jerks are less than 1° in amplitude and rare in healthy controls, but up to 3-4° and more frequent (greater than 10/minute) in PSP.
Note that saccadic intrusions are not specific for PSP and have been described in other conditions, including other parkinsonian syndromes and Friedreich ataxia.
(vv)03 1 Macro Swj 2-1.mp4(tt)
(vv)03 1 Macro Swj 3-2.mp4(tt)
(vv)A03 1 Macro Swj-3.mp4(tt)
(vv)EOA2.mp4(tt)
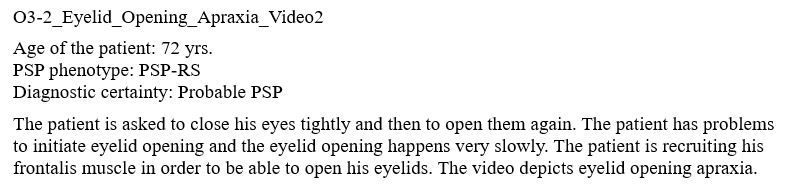
(vv)EOA1.mp4(tt)
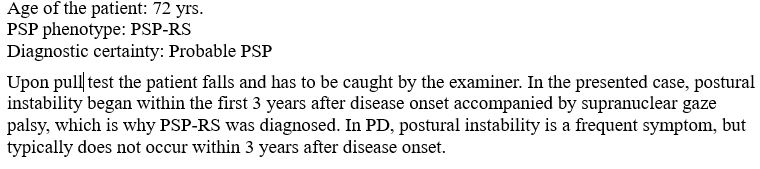
POSTURAL INSTABILITY
DEFINITION: A spontaneous loss of balance while standing, or history of more than one unprovoked fall, within three years after onset of PSP-related features.
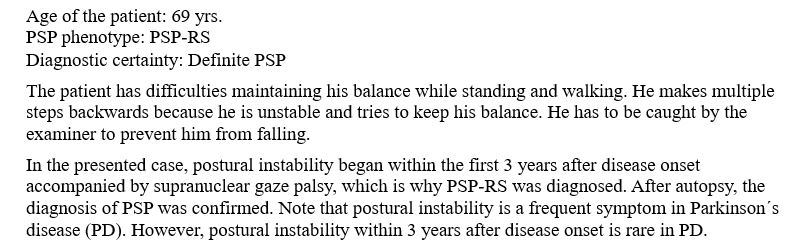
(vv)P1 Mm7.mp4(tt)
DEFINITION: Tendency to fall on the pull-test if not caught by examiner, within 3 years after onset of PSP -related features. The test examines the response to a quick, forceful pull on the shoulders with the examiner standing behind the patient and the patient standing erect with eyes open and feet comfortably apart and parallel, as described in the MDS-UPDRS item 3.12.
For all P2 videos (as for P3 videos): The patient is asked to stand upright and the examiner explains to him how the pull test is performed and that postural responses such as adjustment of the trunk and stepping backward are allowed to regain balance after the pull in order not to fall. The patient should be standing with his feet about shoulder width apart with his weight evenly distributed on both feet. The examiner positions himself behind the patient at a distance that allows recovery space but also to catch the patient if he does not recover balance. The examiner then gives the patient a sudden and firm backward pull to the shoulders.
(vv)P2 Mm8.mp4(tt)
(vv)P2 Mm9.mp4(tt)
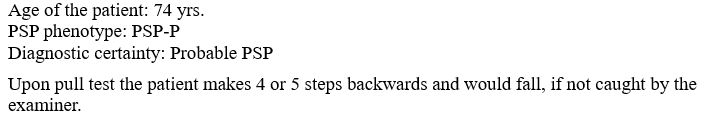
DEFINITION: More than 2 steps backward, but unaided recovery, on the pull-test, within 3 years after onset of PSP-related features.

(vv)P3 more than 2 steps.mp4(tt)
AKINESIA
DEFINITION: Sudden and transient motor blocks or start hesitation are predominant within 3 years after onset of PSP-related symptoms, progressive and not responsive to levodopa; in the early disease course, akinesia may be present, but limb rigidity, tremor, and dementia are absent or mild. [1] While gait freezing is not uncommon in Parkinson´s disease several years after onset of first symptoms, early gait freezing within 3 years is described to be specific for PSP pathology [4]. Gait freezing usually worsens when patients are trying to walk through a narrow space and might not be apparent during a normal neurological exam when the patient is asked to walk. Note that patients with gait freezing are at high risk of falling and appropriate care should be taken.
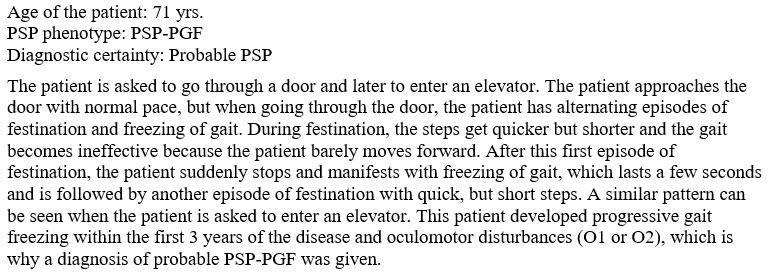
(vv)A1ppgaitfreeze2.mp4(tt)

(vv)A1 Progressive Gait Freezing1.mp4(tt)
DEFINITION: Levodopa-resistance is defined as improvement of the MDS-UPDRS-motor scale by ≤ 30%; to fulfill this criterion patients should be assessed having been given at least 1000 mg (if tolerated) at least 1 month OR once patients have received this treatment they could be formally assessed following a challenge dose of at least 200 mg

(vv)A2parkakrig3.mp4(tt)
DEFINITION: Bradykinesia with rigidity and/or tremor, and/or asymmetric predominance of limbs, and/or levodopa-responsiveness. For A3, the presence of axial predominance and Levodopa-resistance of parkinsonism - as in A2 - is not required. Tremor (at rest or in action) is an optional feature of A3 and may be present in PSP. [1] Note that A3 can be observed in any parkinsonian syndrome and is not specific for PSP. A3 becomes specific only with other signs of PSP, such as slowing of vertical saccades, provides for a diagnosis of PSP.
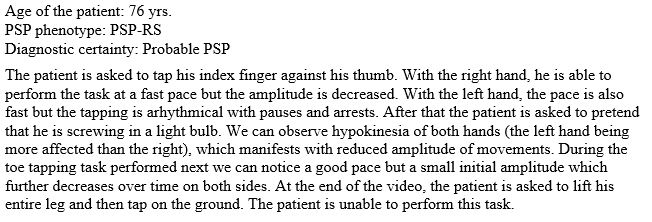
(vv)A3parkasymm5.mp4(tt)
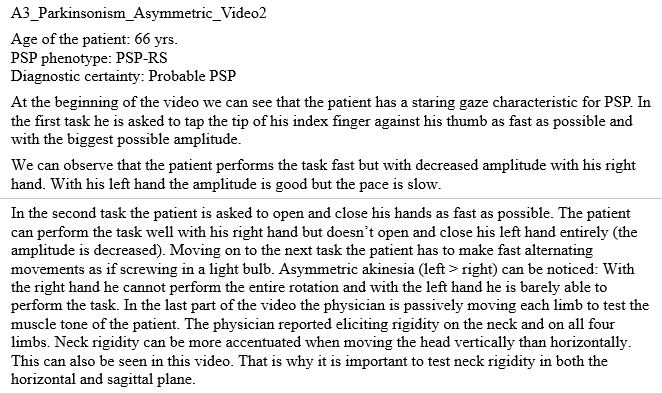
(vv)A3parkasymm 2Nd4.mp4(tt)
(vv)A3parktremor6.mp4(tt)
COGNITIVE DYSFUNCTION
DEFINITION: Loss of grammar and/or telegraphic speech or writing, with spared single-word comprehension, object knowledge and word-retrieval during sentence repetition.
(vv)C11 Nfappa Mm15.mp4(tt)

(vv)C1 1 Nfappa Naming Mm16.mp4(tt)

(vv)C1 1 Nfappa Aud Comprehension Mm17.mp4(tt)

(vv)C11 Nfappa Repetition Mm18.mp4(tt)

(vv)C11 Nfappa Semantic Fluency Mm19.mp4(tt)
DEFINITION: Effortful, halting speech with inconsistent speech sound errors and distortions or slow syllabically segmented prosodic speech patterns,with spared single-word comprehension, object knowledge and word-retrieval during sentence repetition.
(vv)C1 2 Apraxia Of Speech Mm20.mp4(tt)
(vv)C1 2 Apraxia Of Speech Reading 6 Yrs After Onset Mm22.mp4(tt)
(vv)C1 2 Apraxia Of Speech Reading 8 Yrs After Onset Mm23.mp4(tt)
(vv)C1 2 Apraxia Of Speech Reading Mm21.mp4(tt)
DEFINITION: at least 3 of the following features, which have to be persistent (rather than transient).
DEFINITION: Reduced level of interest, initiative and spontaneous activity; clearly apparent to informant or patient.
DEFINITION: Slowed thinking; clearly apparent to informant or patient.
(vv)C2 2 Bradyphrenia Mm24.mp4(tt)
DEFINITION: e.g. reverse digit span, Trails B or Stroop test, Luria sequence (at least 1.5 standard deviations below mean of age- and education- adjusted norms).
(vv)C2 3 Luria Mm25.mp4(tt)
DEFINITION: “D, F, A or S” words per minute (at least 1.5 standard deviations below mean of age- and education- adjusted norms).
(vv)C2 4 Red Phonemic Verbal Fluency Mm26.mp4(tt)
Definition of ‘impulsivity, disinhibition, or perseveration’: Socially inappropriate behaviors, overstuffing the mouth when eating, motor recklessness, applause sign, palilalia, echolalia
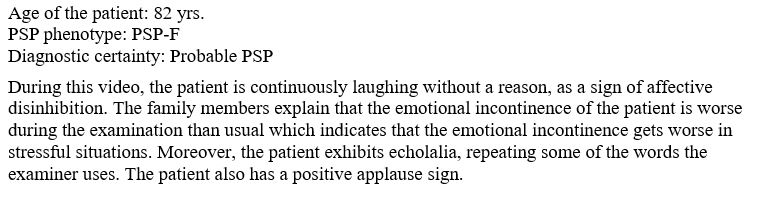
(vv)C2 5 Affective Disinhib Mm27.mp4(tt)
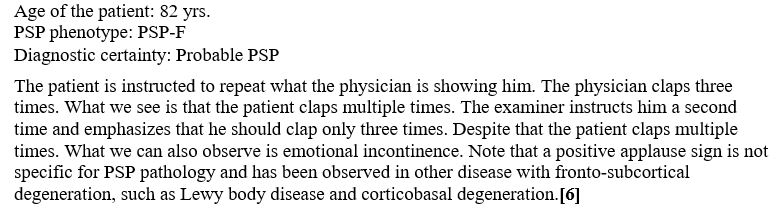
(vv)C2 5 Applause Mm28.mp4(tt)
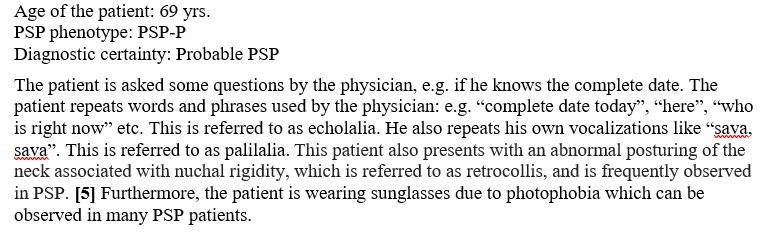
(vv)C2 5 Echo And Palilalia Mm29.mp4(tt)
(vv)Stuff.mp4(tt)
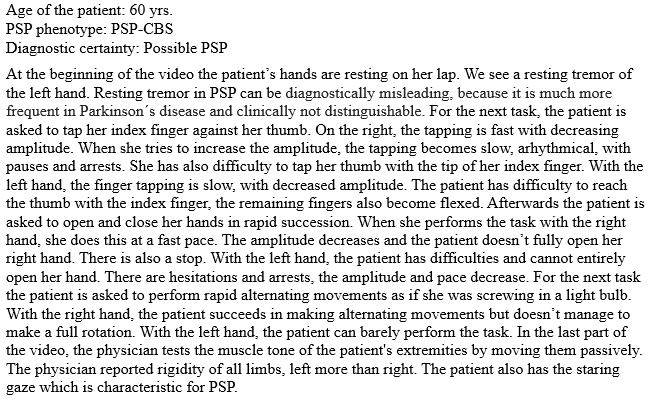
C3 Corticobasal syndrome
DEFINITION: at least 1 sign each from the following 2 groups 1.Cortical signs: a. Orobuccal or limb apraxia; b. Cortical sensory deficit; c. Alien limb phenomena (more than simple levitation); and 2. Movement disorder signs: a. Limb rigidity; b. Limb akinesia; c. Limb myoclonus; d. Limb dystonia (dystonia was unintentionally omitted in the originally publication of the MDS-PSP criteria). The symptoms may be asymmetric or symmetric). [1,7] CBS is not specific to PSP. However, PSP pathology was found in approximately 30% of cases that came to autopsy, apart from corticobasal degeneration (CBD) and Alzheimer´s disease.[7]

(vv)C3 1A Limb Apraxia Mm31.mp4(tt)
(vv)C3 1A Limb Apraxia 22.mp4(tt)
(vv)C3 1B Cortical Sensory Deficit Mm32.mp4(tt)
(vv)C3 1C Alien Limb Mm33.mp4(tt)
(vv)C3 Limb Akinesia3.mp4(tt)

(vv)C3 Limb Myoclonus6.mp4(tt)
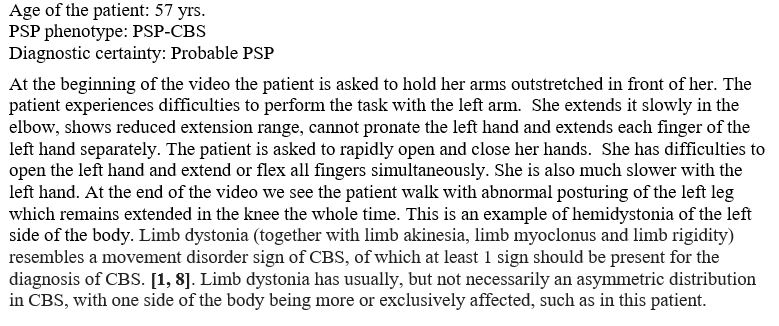
(vv)C3 Limb Dystonia 4.mp4(tt)
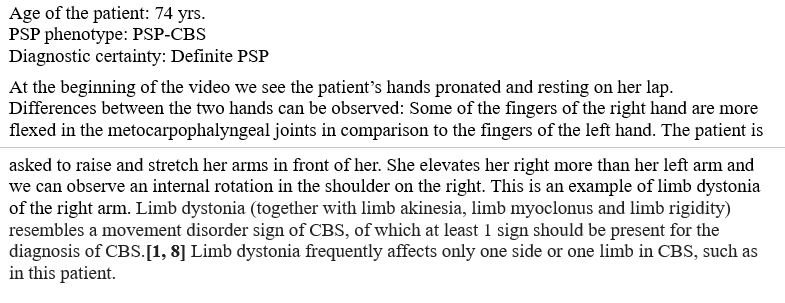
(vv)C3 Limb Dystonia5.mp4(tt)

